What is high-dose melatonin? There’s no objective scientific/medical consensus for what is “high-dose” melatonin.
You might ask several people what they consider to be a high-dose of melatonin – and you might get entirely different answers.
The body endogenously produces between 100 and 300 mcg (micrograms) of melatonin per night (according to a medical doctor on Reddit). (R)
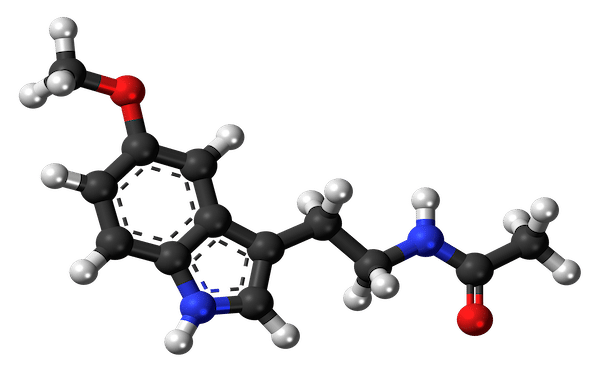
Supplementing with 5 mg of exogenous melatonin would then be delivering between 50-fold and 16-fold more melatonin than is physiologically normative within the body (100-300 mcg).
In this case, one might argue that taking 5 mg is way too much melatonin for most people – and as a result, may cause adverse events induce physiological tolerance with ongoing administration.
However, many people (including melatonin researchers) often fail to consider: (A) oral melatonin bioavailability & (B) individual melatonin pharmacokinetics.
- Poor bioavailability: The bioavailability of melatonin supplements is extremely poor. The absolute bioavailability of oral melatonin documented in a study of 12 healthy volunteers was ~15%. (R)
- Variable bioavailability & plasma concentrations: The bioavailability of oral melatonin supplements can vary significantly between individuals (up to 2.5-fold). Plasma concentrations following oral melatonin administration can vary by up to 37-fold. (R)
Note: Variation in CYP1A2 enzyme activity generally explains most interindividual variability in plasma concentrations – but other factors like co-administered medications, organ function, etc. can also have significant effects (and shouldn’t be discounted).
Let’s consider the average bioavailability of oral melatonin (15%) and evaluate the amount of melatonin from specific oral dosing formats – that ends up biologically active (such as to interact with melatonin receptors in the brain).
Of a 5 mg oral melatonin dose, just 0.75 mg (assuming the 15% bioavailability) ends up generating a physiological effect.
Most probably wouldn’t consider 0.75 mg to be a “high-dose of melatonin” – yet that’s what ends up active (on average).
Sure 0.75 mg is still 2.5-fold greater than 0.3 mg (300 mcg) – but it’s not what most people would consider a high amount.
At a dosage of 10 mg, assuming 15% bioavailability, 1.5 mg of the melatonin actively generates a physiological effect.
1.5 mg is 5-fold more than .3 mg (300 mcg) and an argument could be made that 10 mg is objectively a good minimum threshold level to be considered “high-dose melatonin.”
High-dose melatonin (10-20+ mg melatonin?)
Included below are notes about specific dosage thresholds of supplements that I found on Amazon.
These dosages could be objectively considered “high-dose” melatonin (assuming oral administration).
10 mg Melatonin
This is probably a good minimum amount to be considered “high-dose” melatonin.
This a dose I would personally consider “high-dose” – as it is likely at least 2-fold the amount that the average melatonin user likely takes per night).
- On average, 10 mg provides about 5-fold more melatonin than endogenously produced (and added to the endogenous production).
- 15% of a 10 mg dose is bioavailable – leaving us with 1.5 mg active. The 1.5 mg gets “added” to 100-300 mcg endogenously produced.
- Taking total levels from 100-300 mcg per night to 1.6-1.8 mg per night.
- Even popular supplement manufacturer “NOW” considers “10 mg” melatonin to be “extra-strength” which is synonymous with high-dose or higher-than-average dose.
20 mg Melatonin
Some might argue that 20 mg is a better “threshold” than 10 mg to be objectively considered “high-dose” melatonin.
- Assuming a 15% average bioavailability, 20 mg supplements would yield 3 mg biologically active melatonin per dose – 10-fold more melatonin than is endogenously produced.
- I was able to find various supplement manufacturers on Amazon who sell melatonin in 20 mg tablets/capsules.
60 mg Melatonin
Interestingly, there are multiple supplement companies (Perfect Vitamin & Scientific Health Solutions) that produce melatonin in 60 mg capsules. (Affiliate links used.)
- At 15% average bioavailability, 60 mg supplements would yield 9 mg biologically active melatonin per dose – 30-fold more melatonin than is endogenously produced.
- 60 mg is a level [nearly] everyone would likely objectively consider to be “high-dose” melatonin – and is far above a minimum high-dose threshold dose.
Melatonin Megadose (Explained)
Many people are curious about what differentiates “high-dose melatonin” from “megadose melatonin.”
A melatonin megadose is generally regarded as a dose both: (A) far beyond standard or recommended doses AND (B) beyond even what most would consider “high doses.”
Melatonin megadoses are still technically “high doses” – but the term megadose is used to emphasize the sheer magnitude of the dose.
Many would regard “megadose” as being on a higher dosing tier/echelon relative to “high-dose.”
Okay, so what dosage would be considered a melatonin megadose?
Once again, this is somewhat subjective – and probably depends on who you ask.
Some might argue that anything above 20 mg is a “megadose” whereas others might suggest that the dosage needs to be at least 50 mg or 100 mg.
In early research of exogenous melatonin (1960s, 1970s, 1980s, early 1990s), it was common to test large oral doses of melatonin.
- Arutyunyan et al. (1964): 200 mg to 1200 mg
- Anton-Tay et al. (1971): 100 mg (IV infusion)
- Cramer et al. (1974): 50 mg (IV infusion)
- Lerner & Norlund (1975): 1000 mg (28 days)
- Carman et al. (1976): 200 mg to 1200 mg (per day)
- Lieberman et al. (1986): 240 mg
- Valcavi et al. (1987): 500 mg
- Waldhauser et al. (1987): 80 mg to 240 mg
- Waldhauser et al. (1990): 80 mg
At the time, these were probably considered “high doses” – not necessarily megadoses (but I could be incorrect in this thought.)
These days, I suspect that most people and melatonin researchers would consider the aforementioned doses to be “megadoses.”
I suspect that perception of what is a “high” melatonin dose has changed (slightly or significantly) throughout the years given that modern research doesn’t typically involve such large melatonin boluses like decades of the past.
I think that a good minimum threshold dose to be regarded as a melatonin megadose is 100 mg.
Why? Because 100 mg is delivering 10-fold more melatonin to the body than 10 mg (a dosage that many would already consider to be “high”).
(That said, I’d understand if someone pushed for a higher level such as 500-1000 mg or 0.5-1 gram as being the minimum threshold dose to be regarded as a “melatonin megadose.”)
This fits the criteria of megadose: (A) well-beyond a standard dose AND (B) beyond what most would consider a “high dose.”
Many unfamiliar with melatonin might panic (fearing respiratory depression, organ damage, and/or death) following ingestion of a megadose quantity, but thankfully, melatonin is a very safe substance (assuming taken alone – without other drugs in one’s system).
Note #1: I do NOT endorse taking high-dose or megadose melatonin without verifying safety with a medical professional.
Note #2: The dosing definitions are specifically for standard melatonin supplements taken orally – not for other formats or routes of administration. (Other routes of administration will have different bioavailability and there may be atypical oral melatonin formats with higher bioavailability).
What is the highest dose of melatonin tested on humans?
I’ve read a boatload of melatonin papers, and I’ve found some pretty high doses used – and cannot be sure that I’ve definitively found the “highest.”

The highest dosing I was able to find comes from an observational study published by Papavasiliou et al. (1972). (R)
Study participants: 11 patients with Parkinsonism who received “high dose” melatonin (about half also received concomitant Levodopa).
Each of the doses listed below corresponds with one of the 11 participants in the trial. I’ve listed the doses in descending order (highest to lowest).
- 6 grams per day for 35 days: A patient in this study administered 6.6 grams (6600 mg) of melatonin per day for 35 days. This is the highest dose of melatonin tested on a human that I could find (and for a pretty significant duration to boot).
- 4 grams/day (34 days)
- 5 grams/day (31 days)
- 5 grams/day (23 days)
- 2 grams/day (26 days)
- 2 grams/day (25 days)
- 1 grams/day (28 days)
- 9 grams/day (21 days)
- 6 grams/day (27 days)
- 3 grams/day (15 days)
- 3 grams/day (16 days)
You’re probably wondering, were there any side effects from such large melatonin doses?
Yes. Isolated incidences of: cutaneous flushing, abdominal cramps, diarrhea, scotoma, and migraine headaches.
Because Levodopa was coadministered in about half of the patients, it’s unclear as to whether it may have caused (rather than melatonin) or contributed to (along with melatonin) these side effects.
The 2 patients taking the highest dosages (6.6 grams/day & 5.4 grams/day) experienced daytime sleepiness (i.e. somnolence) – as did an additional 4 patients on lower doses.
What’s the highest dose melatonin tested on animal models?
I haven’t spent much time digging into the animal data. A cursory search led me to StatPearls (a source that I like and endorse – that provides a general overview of various substances). (R)

800 mg/kg: Apparently researchers haven’t been able to discover an LD50 (lethal dose for 50% of subjects) for melatonin in animals. A dosage of 800 mg/kg was NOT fatal.
Although this dosage cannot be directly extrapolated to humans, let’s determine how much this would be for an average adult American male (89.7 kg).
This would equate to taking a melatonin dose of 71.76 grams without dying (and I’m not even sure if there were significant adverse events).
Quick Overview (High-dose vs. megadose vs. supraphysiologic dose vs. overdose)
High-dose melatonin: A dose above a “standard” or conventional dose. For melatonin this is about 10 mg and up.
Melatonin megadose: This is a dose far above a conventional dose – and above what most high-dose users would consider. For melatonin, this is probably something like 100 mg and up.
Supraphysiologic dose of melatonin: This is a dose above levels that are naturally present within the body. A supraphysiologic dose for melatonin is extremely low (as endogenous nightly secretions are likely between 100-300 micrograms).
Melatonin overdose: An “overdose” of melatonin occurs whenever someone takes more than their usual dose (either intentionally or unintentionally). Read: Melatonin Overdose.
High Dose Melatonin Effects (Common)
Individuals taking high-dose melatonin are most likely to experience general tiredness or sleepiness as a result of the dose.
- Drowsiness, sleepiness, tiredness
- Fatigue & lethargy
- Disorientation (mild to moderate)
- Nightmares and/or vivid dreams
- Vision changes (e.g. scotoma)
- Skin flushing (warm sensations)
- Abdominal cramps, diarrhea, gastritis
In most cases, high-dose melatonin will simply cause mental fatigue and sleepiness. I’m not going to document all potential adverse events of high-dose melatonin, but will mention a couple to watch for.
High-Dose Melatonin (Adverse Reactions to Watch For)

Hypotension
It is thought that melatonin could cause dangerously severe hypotension in some cases.
It may be prudent to monitor blood pressure anytime taking high levels of melatonin.
(Look out for orthostatic hypotension as well wherein you feel dizzy after standing up from a seated/prone position).
Memory lapses
Melatonin might cause memory lapses for some individuals – such that they forget what happened while under the influence of melatonin.
Circadian dysregulation
This may not occur until several weeks or months after you began taking melatonin.
Essentially, melatonin stops delivering a beneficial effect because a high concentration has accumulated in your body (for various reasons).
Best course of action for this is to stop melatonin for 2 weeks then reinstate usage with a low dose (0.3 mg) indefinitely.
Read: Low dose melatonin.
Note: If you’re taking melatonin with another substance in your system – do not automatically assume that the effects you’re experiencing are from melatonin.
What is the highest dose of melatonin I’ve ever taken?
I could be inaccurate in my recollection (as this was over a year ago), but I think I administered about 50 mg melatonin within a ~12-hour window.
The melatonin was administered along with other substances – mostly magnesium (threonate & citrate).
I took 30 mg melatonin about 30 minutes before going to bed. Then each of the 2 times I woke up in the middle of the night I took an additional 10 mg.
In any regard, what were the subjective effects I experienced from taking high-dose melatonin?
(I’ve taken high dose melatonin multiple times and am not sure of the exact amounts that I administered – but think that I may have taken more than 50 mg.)
I suspect my reactions are probably similar for most people taking equipotent doses…
- Sleepiness & higher sleep inertia/drive (relative to lower melatonin)
- Altered state of consciousness (shifted perception)
- Depersonalization (very modest)
- Relaxation (physical & mental)
- Subjectively improved sleep relative to without
What was the point of taking such a high amount of melatonin in a short period of time?
Partly because I thought it would help my body recover from hyperarousal and Acute Stress Disorder.
Taking melatonin at high-doses liberally (such as popping 5-10 mg every time I’d wake up in the middle of the night) definitely helped… subjectively I felt as though my sleep quality was much higher relative to lower doses.
Note: I cannot be sure that all of these effects were solely from melatonin – as other supplements were co-administered. That said, my melatonin dosage was significantly higher than usual.
Are high doses of melatonin “better” for certain health/medical conditions?
Probably. High-dose melatonin is thought to activate MT1 & MT2 receptors more substantially than lower-dose melatonin – such that they end up “oversaturated” (which may generate uniquely advantageous neurobiological effects that cannot be attained with lower doses).
High-dose melatonin and/or high levels of specific metabolites resulting from a high dose – may also exert additional effects such as: (1) inhibition of CaM-mediated nNOS activation & (2) modulation of ion channels.
Perhaps the most medically-relevant benefits of high-dose melatonin include: (1) anti-oxidative & (2) anti-inflammatory actions – which are orders of magnitude greater than would result from low-dose and even standard-dose melatonin.
(The anti-oxidative and anti-inflammatory actions of melatonin may be dose-dependent – such that low doses aren’t nearly as beneficial as high doses if the goal is to significantly reduce both oxidative stress and inflammation.)
I would also surmise that other melatonin actions such as: cellular/mitochondrial protection and immunomodulation are significantly more pronounced (and probably medically relevant) at high doses and megadoses – relative to standard and low doses.
Although circadian regulation may be a benefit of high-dose melatonin, some speculate that this benefit may be transient – particularly if administered chronically and/or to inefficient metabolizers (e.g. underactive CYP1A2 enzyme).
When High-Dose Melatonin May Be Best…
Included below is a list of medical conditions and scenarios in which high-dose melatonin may be more advantageous than low-dose melatonin.

Radiation poisoning
If exposed to radiation, high-dose melatonin is worth considering as a potential adjunct treatment.
I personally think there’s little to no risk of using high-dose melatonin if you’re a victim of radiation poisoning – particularly in the immediate/acute aftermath of exposure.
I wouldn’t really waste time messing with low dose melatonin here.
- Vijayalaxmi et al. (1998): A single oral dose of 300 mg melatonin significantly reduced DNA-damage from 100 cGy and 150 cGy gamma radiation – relative to no melatonin. (R)
Liver surgery adjunct
As I’ve mentioned, melatonin protects organs – including the liver from damage (e.g. hepatotoxicity). This protection may be more pronounced at high doses.
- Nickkholgh et al. (2011): A single preoperative, high-dose of melatonin (via enteral administration) is effectively absorbed, safe, and well-tolerated in patients undergoing major liver surgery. (R)
- A randomized controlled trial assigned 50 patients to receive either: melatonin (50 mg/kg BW) or microcrystalline cellulose (placebo).
- Melatonin was effectively absorbed and recipients exhibited high serum concentrations (avg. = 1142.8 ng/mL) vs. controls (avg. = 0.3 ng/mL).
- Melatonin recipients exhibited lower postoperative transminases and a trend for a shorter ICU stays.
Nerve injuries
In the aftermath of a nerve injury, it appears as though high-dose melatonin is superior to low-dose melatonin for the acute attenuation and reversal of nerve damages.
- Shokouhi et al. (2008): Compared the effects of low-dose melatonin (10 mg/kg) high-dose melatonin (50 mg/kg) vs. a placebo (diluted ethanol) – on ultrastructural changes and lipid peroxidation – following blunt peripheral nerve injury in rats. (R)
- Trauma analyses discovered dose-dependent attenuation of nerve lipid peroxidation and ultrastructural changes.
- Low-dose melatonin reduced trauma-induced myelin breakdown and axonal changes in the sciatic nerve – whereas high-dose melatonin almost entirely neutralized any ultrastructural changes.
- (In other words, high-dose melatonin was significantly more therapeutic in attenuation of nerve damage – than low-dose melatonin… but even low-dose melatonin was significantly more therapeutic than a placebo.)
- Conclusion: High-dose melatonin exerts potent neuroprotective effects and can preserve peripheral neural fibers from lipid peroxidative damage following blunt trauma.
Drug dependence & neurotoxicity
Individuals who’ve developed drug dependence (physical and/or psychological), are addicted to certain drugs, and/or regularly use high-doses of potentially toxic drugs might benefit from high-dose melatonin.
Why? Certain drugs such as MDMA, cocaine, and amphetamines (e.g. methamphetamine) are likely neurotoxic – particularly when taken regularly and/or at high-doses. (R)
Assuming melatonin can counteract or prevent neurotoxicities – the degree of its therapeutic effect may be contingent upon its dose.
Preliminary data would lead me to believe that high-dose melatonin should be more efficacious (even if marginally so) than low or standard dose melatonin – for counteracting neurotoxicities.
Why? Neurotoxicities are associated with, and can be exacerbated by, high-inflammation and oxidative stress.
High-dose melatonin (theoretically) should reduce inflammation and oxidative stress more substantially than low-dose melatonin.
Itzhak et al. (1998) found that (in animal models) high-dose melatonin (10 mg/kg) prevented methamphetamine-induced depletion of: dopamine AND dopamine transporter (DAT) binding sites – AND diminished drug-induced behaviors. (R)
Feng et al. (2013) found that (in animal models) melatonin dose-dependently prevented development of morphine-induced behavioral sensitization and analgesic tolerance… higher doses were more effective. (R)
Amyotrophic lateral sclerosis (ALS)
High-dose melatonin (300 mg/day) administered chronically (up to 2 years) appears to decrease the severity of ALS in animal models.
- Weishaupt et al. (2006): In mouse models of ALS, high-dose melatonin: (A) delayed disease progression and (B) extended survival – likely by significantly reducing oxidative stress (as evidenced by normalization of serum protein carbonyls – from a previously elevated state – following melatonin treatment). (R)
Duchenne muscular dystrophy (DMD)
Administration of high-dose melatonin (70 mg/day) may prove therapeutically beneficial for patients with DMD by decreasing hyperoxidative and inflammatory processes AND limiting the process of muscle degeneration.
- Chahbouni et al. (2010): 10 DMD patients aged ~12.8 were treated with melatonin (60 mg at 9:00 PM – plus 10 mg at 9:00 AM) for 9 months. (R)
- Measures: Plasma lipid peroxidation (LPO); nitrites (NOx); IL-1b; IL-2; IL-6; TNF-alpha; IFN-gamma; and plasma markers of muscle injury (evaluated every 3 months).
- Results: Melatonin administration significantly decreased levels of: LPO; NO(x); and cytokines in plasma (at 3 months, with additional reductions at 9 months) – and significantly reduced markers of muscle injury.
- Conclusion: High-dose melatonin (total of 70 mg/day) substantially reduces DMD-related hyperoxidative and inflammatory processes (which should help minimize/slow muscle degeneration.)
Sleep maintenance (?)
Although low-dose melatonin is more than sufficient for sleep induction (and reducing sleep onset latency) – it may be inferior to high-dose melatonin for sleep maintenance.
Select studies suggest that high-dose melatonin (50-100 mg) might be better for sleep maintenance. (R)
Oral contraceptive (?)
High-dose melatonin (up to 300 mg/day) may be useful as a standalone or adjunct oral contraceptive (such as with progestin norethisterone).
It is unclear as to how effective high-dose melatonin actually is as an oral contraceptive in humans (as not much testing has been done beyond studies in the early 1990s). (R)
- Voordouw et al. (1992): Melatonin and melatonin/progestin norethisterone combinations inhibited ovarian function in 32 women over a 4-month span – leading researchers to conclude that melatonin may prove useful as an oral contraceptive. (R)
Protection against toxicities
High-dose melatonin may provide significant protection against: (1) Cytotoxicity; (2) Neurotoxicity; (3) Genotoxicity; (4) Drug-induced toxicities; (5) Infection-induced toxicities; (6) Radiation-induced toxicities; and more (e.g. ototoxicity, ocular toxicity, nephrotoxicity, hepatotoxicity, etc.);
How does it do this? Primarily by significantly decreasing: (A) oxidative stress & (B) inflammation.
(Don’t believe me? Just Google melatonin for a specific “toxicity” – and you’ll likely find a study supporting its usage.)
If you were recently exposed to one or more toxic insults, I would guess that: (1) there’s a time-sensitive window to achieve therapeutic effects from melatonin (such that the sooner it’s taken – the better) AND (2) higher doses are significantly better than lower doses at attenuating toxicities (but any dose is probably better than no melatonin).
Cancers & carcinogens (?)
There’s preliminary evidence to suggest high-dose melatonin may be beneficial in: (1) the treatment of various cancers (when administered as an adjunct); (2) protecting the body from cancer formation; (3) preventing or slowing the growth/spread of existing cancers.
- Gurunathan et al. (2021): Considerable evidence from experimental studies suggest melatonin can be used to prevent and treat cancer. (R)
- Melatonin mitigates the pathogenesis of cancer by directly affecting carcinogenesis and indirectly disrupting the circadian cycle.
- Melatonin is nontoxic and exhibits an array of beneficial anti-cancer effects, including: (1) apoptotic; (2) antiangiogenic; (3) antiproliferative; (4) metastasis-inhibitory.
- Combining melatonin with conventional anti-cancer agents improves drug sensitivity to cancers (i.e. likelihood the drugs will eliminate the cancer) – including solid and liquid tumors.
- Authors suspect potential benefits of melatonin in: lung, breast, prostate, colorectal, skin, liver, cervical, and ovarian cancers.
- Wang et al. (2012): Melatonin (20 mg/day) as an adjunct therapy for cancer led to substantial improvements in tumor remission, 1-year survival, and alleviation of radiation/chemotherapy side effects. (R)
Cognitive enhancement & preservation
Melatonin may be useful as a substance to enhance cognition (particularly among persons with age-related cognitive decline) – and may prevent or delay onset of neurodegenerative conditions.
- Cardinali et al. (2012): “Melatonin can be a useful add-on drug for treating mild-cognitive impairment in a clinic environment.” (R)
- Data from a series of 61 patients with mild-cognitive impairment (MCI) who received 3-24 mg melatonin at bedtime (15-60 months) suggest melatonin significantly improves cognition.
- “Studies in MCI with melatonin doses in the range of 75-100 mg/day are further warranted.”
Although numerous studies have found standard doses (e.g. 1-5 mg melatonin) effective for the treatment of cognitive decline/impairment – other research supports the use of high doses.
It’s unclear as to whether melatonin dosing discrepancies (e.g. low, standard, high) yield significantly different: (A) magnitudes of cognitive enhancement and/or (B) effects on specific cognitive domains.
- Cardinali (2019): “Melatonin combines both chronobiotic and cytoprotective properties” – and thus may be capable of preventing or delaying neurodegenerative disorders, but prevention/delay may only occur at high doses. (R)
- Melatonin reverses the low degree inflammatory damage observed in neurodegenerative disorders and aging.
- Experimental models of Alzheimer’s disease (AD) and Parkinson’s disease (PD) show that melatonin prevents neurodegeneration.
- Melatonin increases removal of toxic proteins via the brain’s glymphatic system.
- Calculations derived from animal research suggest cytoprotective doses of melatonin are high (range of 40-100 mg/day).
- Unfortunately, there are no large-scale studies that’ve investigated such a high dose of melatonin as a protector from neurodegeneration.
- Sumsuzzman et al. (2021): Meta-analysis indicates that melatonin is effective in the treatment of mild stage Alzheimer’s disease (AD). (R) Dosages administered in trials included within the meta-analysis ranged from 5 mg to 80 mg – but it remained unclear as to whether high-doses differ in effect from lower doses.
Infections (Viral & Bacterial)
High-dose may prove useful in the prevention and treatment of various infectious diseases – as a standalone (in prophylaxis) and adjunct (in treatment).
Common infections for which melatonin appears beneficial include: (1) COVID-19 (2) Tuberculosis; (3) Influenza.
How would melatonin be beneficial in the management of infectious disease? It appears to reduce the severity and improve outcomes in sepsis (as was discussed).
Its pleiotropic actions include: antioxidant effects; anti-inflammatory effects; mitochondrial, cellular, organ protection; modulation of nitric oxide; circadian regulation; and immunomodulation – all of which could prove beneficial in infectious disease.
- He et al. (2021): Melatonin could be a useful treatment for various pathogenic bacterial infections – but may only be effective at “very high concentrations.” It may modulate various signaling pathways, including: NF-kB; STAT-1; Nrf2; NLRP3; MAPK; and TLR-2/4. (R)
- S. aureus: 10 mg/kg. (Reduced expression of LPO, CAT, iNOS, COX-2, TNF-a, IFN-y, IL-6, CRP, and increased SOD & GSH.)
- S. pneumoniae: 2 mg/mL. (Suppressed bacterial growth at high concentration – a.k.a. was bacteriostatic.)
- E. coli: 10 mg/kg or 1nM. (Reduced LPO, CAT, iNOS, COX-2, TNF-a, IFN-y, IL-6, CRP, and increased SOD & GSH.)
- H. pylori: 5 mg or 3 mg. Increased effectiveness of H. Pylori elimination and enhanced duodenal ulcer recovery.
- Pneumonia: 100 mg/kg. Counteracted neurocognitive damage inhibiting microglia activation – and reduced proinflammatory cytokine levels.
- Pasteurella multocida (P52): 100 mg/kg. Exogenous melatonin 4-hours post-vaccination enhanced immune responses in rats.
- Pasteurella multocida (PmCQ2): 30 mg/kg; 60 mg/kg; 120 mg/kg. Inhibited excessive inflammation resulting from macrophages.
- Wiid et al. (1999): Melatonin can cause at least a 3-fold increase in the effectiveness of isoniazid against tuberculosis. (R)
- “Melatonin, being substantially hydrophobic, may locate itself in the mycobacterial cell wall, causing destabilization and enhanced permeability for molecules such as INH (isoniazid).”
- Ozkan et al. (2012): “We believe that the treatment of TB patients with melatonin might result in a wide range of health benefits including improved quality of life and reduced severity of infection.” And… “Supplementation with melatonin may be considered as an adjunctive therapy to classic treatment of pulmonary TB.” (R)
- DiNicolantonio et al. (2021): Melatonin supplementation may have general utility for the prevention and treatment of RNA virus infections such as COVID-19 and influenza. (R)
- Anderson & Reiter (2020): High-dose melatonin may be useful in the treatment of COVID-19 and influenza. (R)
- “Melatonin is actively inhibited by most viruses, indicating its importance in the regulation of viral infections.”
- “A further benefit of melatonin in the management of influenza and COVID-19 arises from its utility in the management of preexisting medical conditions associated with viral-linked fatality.”
- “Extrapolating from preclinical data would suggest that melatonin doses as high as 500 mg may be necessary to dampen the initial cytokine storm” (associated with COVID-19).
Personally, I’d love to see high-dose melatonin investigated in the treatment of infections (particularly tuberculosis and nontuberculous mycobacteria) – as it:
- Is nontoxic.
- Generally minimizes toxicities (infection and medication-related).
- May act synergistically with conventional treatments.
- May elicit its own bacteriostatic/bactericidal effect at certain doses.
- May modulate the immune system in ways that enhance innate immunity.
Stroke recovery & prevention
Although low and standard doses of melatonin do NOT appear effective in RCTs for the treatment of neurobiological damage resulting from stroke – high-doses may be beneficial (but haven’t been well-studied in humans).
- Ramos et al. (2020): “Calculations derived from animal studies revealed that translational doses to humans were substantially higher than those employed in RCTs.” (R)
In other words: Existing studies evaluating melatonin as an acute therapy for stroke-induced brain damage administered doses far too low [based on animal research in which melatonin proved beneficial].
Sepsis
Sepsis (a life-threatening condition caused by infection) affects 30 million people worldwide and causes 6 million deaths each year.
High-dose melatonin may prove useful as an adjunct in the treatment of sepsis. (R)
If I ever got sepsis, I’d hope that a doctor would administer megadose melatonin (assuming no interactions with conventional medications) – to minimize toxicities from both sepsis AND medications – while enhancing immune function.
- Biancatelli et al. (2020): High-dose melatonin may improve sepsis via numerous mechanisms (including but not limited to):
- Antioxidant effects
- Anti-inflammatory effects
- Prevention of mitochondrial dysfunction
- Prevention of hepatic injury
- Prevention of cardiomyopathy
- Inhibition of nitric oxide
- Prevention of sepsis-induced brain dysfunction
- Immune system enhancement
- Circadian regulation
Anti-aging (?)
It has been speculated that high-dose melatonin may delay aging and/or prevent accelerated aging in humans – particularly when administered at high doses.
- Armstrong & Redman (1991): Melatonin’s anti-aging properties may be related to: (A) immune system enhancement; (B) anti-stress properties (via brain opioid system); (C) reversing age-related amplitude reductions in the circadian pacemaker system. (R)
- “Stability of the circadian system correlates with its amplitude and loss of circadian amplitude produces lability which, in turn, leads to internal temporal disorder – a precursor of disease states.”
- Bubenik & Konturek (2011): Hypothesize that: (A) reduction of melatonin levels with age contributes to the aging process AND (B) daily intake of melatonin before bed might delay aging. (R) The logic?
- Melatonin is a strong antioxidant (scavenging free radicals) which protect the body from the effects of noxious compounds.
- Thus far, the only proven way to extend lifespan has been 40% calorie reduction (prolongs life of mice, rats, dogs, and monkeys by ~30-50%).
- Fasting in animals significantly increases production of gastrointestinal tract (GIT) melatonin – and may be a key mechanism by which fasting prolongs life (delaying aging).
- Nightly administration of melatonin (e.g. before bed) has potential to achieve the same neurobiological effect as fasting – protecting individuals from age-related disease.
- There is a large group of individuals who strongly believe that daily melatonin administration is the “fountain of youth.”
- Kleszczynski & Fischer (2012): Evidence suggests that high-dose melatonin may prevent skin aging in humans when applied topically. (R)
- Melatonin counteracts generation of reactive oxygen species, mitochondrial damage, and DNA damage – following exposure to UV-solar rays.
- This paper is advocating for topical administration of high-dose melatonin (i.e. directly on the skin) rather than oral administration (as oral administration has low bioavailability and won’t reach significant levels in skin tissue.)
- Hardeland (2019): Melatonin may delay aging and prevent age-related diseases by: modulating inflammation & immune function – and regulating the circadian rhythm. (R) The aforementioned actions may have downstream effects on:
- Nitric oxide release
- SIRT1 activation
- Cyclooxygenase-2 inflammasome NLRP3
- Gasdermin D
- Toll-like receptor-4
- mTOR signaling
- SASP-mediated cytokine release
- Amyloid-beta toxicity
- Nrf2 (upregulation)
- NF-kB (downregulation)
- IL-4 & IL-10 release
- Macrophage & microglia polarization (M2 phenotype)
- mRNAs & mRNAs of inhibitor proteins
Important clarifications regarding high-dose melatonin…
Do NOT assume that high-dose melatonin should be automatically used for the conditions listed above just because some preliminary evidence suggests that: (1) it provides a therapeutic effect OR (2) it’s effective in animal models.
Evidence that high-dose melatonin “may work” for a certain medical condition or scenario may be of low-quality (as a result of a small sample, poor trial design, or other limitations).
Additionally, just because high-dose melatonin appears therapeutic in animal models of conditions (e.g. sciatic nerve injury, stroke, etc.) – does NOT mean that this can be extrapolated to humans.
Nonetheless, risk vs. reward associated with trying high-dose melatonin in certain medical scenarios – would generally favor a melatonin trial (as risks are almost nonexistent and rewards are potentially significant.)
Understand that it’s unknown as to what average dose or dosing range melatonin is optimal for specific medical conditions – as melatonin hasn’t been proven significantly efficacious for much of anything (beyond insomnia in older adults).
Furthermore, optimal doses of melatonin may be somewhat individually-specific given interindividual differences in melatonin pharmacokinetics (i.e. absorption, metabolism, distribution, plasma concentrations, elimination).
The degree to which high-dose melatonin differs in efficacy relative to standard-dose or low-dose melatonin for any medical condition remains unknown in humans.
That said, because: (A) melatonin is a cheap supplement that cannot be patented (such that there’s no financial incentive to study it) AND (B) high-doses are not typically evaluated in humans – the current science lacks a complete understanding of melatonin’s therapeutic potential.
As a result, we must consider that high-dose melatonin might be very effective in certain medical scenarios (as a standalone or adjunct) – including scenarios that haven’t yet been studied or discussed in the scientific literature.
What do I think about high-dose melatonin?
It’s probably unfair to conclude (as of 2021) that high-dose melatonin is automatically more therapeutic than low-dose melatonin for any particular medical condition.
Even in some studies that administered high-dose melatonin (e.g. DMD at 70 mg/day) – there wasn’t a lower-dose melatonin group for comparison to know whether high-doses are more therapeutic.
In my opinion, there’s significantly more upside to administering high-dose melatonin (relative to standard and low-dose melatonin) in many cases (with a few exceptions such as preventing amikacin-induced ototoxicity).
Why? Because I hypothesize that the magnitude of anti-oxidative and anti-inflammatory effects are dose-dependent (up to a certain extent) – and that they should be more pronounced with higher plasma melatonin concentrations.
I don’t know of any major downsides associated with administering megadose/high-dose melatonin in an emergency scenario (assuming no interactions with other medications).
Conditions for which I’d probably consider using high-dose melatonin (assuming my doctor says it’s safe):
- Abnormally high systemic inflammation (for whatever reason)
- Abnormally high oxidative stress (for whatever reason)
- Duchenne Muscular Dystrophy (70 mg/day)
- Drug dependence & withdrawal syndromes
- Liver surgery (50 mg/kg BW)
- Nerve injuries
- Sepsis & infections
- Post-stroke
- Amyotrophic lateral sclerosis
- Certain cancers
- Mild neurodegeneration
- Sleep maintenance
That said, I’d probably work with a doctor to determine how the melatonin is affecting: (A) relevant biomarkers; (B) sleep & circadian rhythm; and (C) performance (physical & cognitive).
If I were a slow melatonin metabolizer, and wanted to use melatonin chronically, I may use a much lower dose of melatonin (particularly because high-doses would accumulate and inevitably dysregulate the circadian rhythm).
In the acute aftermath of something like a stroke – I wouldn’t be too concerned about circadian dysregulation from high-dose melatonin (because it usually takes a few weeks to set-in).
Divergent Importance of Chronobiological Considerations in High & Low Dose Melatonin Therapies (2021)
Hardeland (2021): (R)
High-dose melatonin (up to several hundred milligrams) may be unsuitable for chronobiological purposes (relative to low-dose melatonin) as it may dysregulate circadian rhythms – it might be significantly better at reducing oxidative stress and inflammation.
Significantly reducing oxidative stress and inflammation may be particularly relevant in scenarios like sepsis and viral infection – and may only be achieved with large melatonin doses.
Hardeland advocates for high-dose melatonin in specific cases & shares his logic:
- “The aim of protecting lives against acute potentially deadly pathologies fully justifies the use of high doses, regardless of whether the treatment may disturb the circadian system.”
- “Perturbations of biological clocks may not be as severe as one might think as long as melatonin is only regarded as a single component of the circadian system.”
- “There is no good reason for believing that oscillators would be stopped by high melatonin (i.e. a compound that shifts clocks or extends periods by only a few hours).”
- “Melatonin’s additional advantage of detoxifying highly reactive and damaging intermediates should not be underrated – a property that is not shared by synthetic melatonergic drugs (e.g. ramelteon).”
- “Moreover, the supreme tolerability of melatonin must be appreciated.”
Melatonin is extremely tolerable, often causing no serious side effects, and is considered non-toxic even at megadoses.
In other words – in certain circumstances/situations, the potential benefits of using high-dose melatonin massively outweigh the potential cons.
Note: There are probably other scenarios in which high-dose melatonin might be beneficial. I just listed some that I could think of off the top of my head.
High-dose melatonin (Pros vs. Cons)
It should be mentioned that using “high-dose melatonin” may come with both benefits and drawbacks.
For example, in a life-threatening scenario (e.g. sepsis), acute administration of high-dose melatonin may have significant benefit:
- Immunomodulation.
- Synergism with conventional treatments.
- Protection against toxicities (from infection & medications).
- Lowering free radicals/oxidative stress & inflammation.
However, consistent and chronic administration of high-dose or megadose melatonin (in the aforementioned scenario) may dysregulate the circadian rhythm (to some extent) and cause excessive fatigue/sleepiness and worsening of sleep quality.
Although circadian dysregulation and/or excessive fatigue/sleepiness may be “drawbacks” associated with using high-dose melatonin – most would agree the benefits outweigh the drawbacks in this specific case (assuming melatonin works as hypothesized.)
On the other hand, taking “high-dose melatonin” over a long-term: (A) for cancer prevention; (B) to keep inflammation as low as possible; or (C) as an anti-aging strategy – may not be as logical.
At high-doses, some individuals may not realize that they’re accumulating melatonin (due to massive doses and possibly inefficient metabolism) – such that levels remain high 10+ hours post-administration or during daytime, thus causing: circadian dysregulation; low energy; excessive daytime fatigue/sleepiness; impaired concentration/cognition; low motivation; low productivity; etc.
Unless there’s a medical need for high-dose melatonin, it’s probably smart to stick with the “minimal effective dose” (MED) unless you’re fully aware of potential risks and aren’t subjectively/objectively noticing any side effects (e.g. cognitive deficits; daytime fatigue; etc.).
Would I recommend “high-dose melatonin”?
It depends – on the specific person and whether they’d likely benefit.
If you have poor CYP1A2 metabolism or kidney/liver impairment, high-dose melatonin should NOT be used unless there’s an urgent medical need for it (e.g. adjunct in sepsis or cancer) – as it will likely accumulate rapidly and dysregulate your circadian rhythm (probably within 4 weeks).
If you plan on consistently using high-dose melatonin or megadose melatonin – know: (1) exactly why you’re using it (have some rationale); (2) the specific dose to take; (3) the specific duration for which you’ll use it; (4) the optimal administration timing (e.g. at night); and (5) ideal administration frequency (e.g. daily).
At this time, there isn’t strong evidence to formally endorse the usage of high-dose or megadose melatonin for any medical condition – particularly over the long-term (this may change in the future if high-dose melatonin research gets funded.)
If you’re dead-set on taking high-dose melatonin for the long-term, it would be smart to work with a medical doctor who supports your decision – and get blood work done (e.g. at pre-melatonin baseline, first few months of use, then every 6 months if things are going well).
What type of blood work should you get done?
I’d personally want a medical doctor to evaluate: CBC, lipids, hormones, vitamins/minerals, inflammation, and have an immunologist review my immune function (to determine whether/how the melatonin may have influenced function).
If high-dose melatonin is making you feel depressed, unproductive, or drowsy all day – it’s probably not worth taking for a long-term.
Always review how you subjectively feel and perform (cognitively and physically) – at various intervals (e.g. daily, weekly, monthly – if you’re a chronic high-dose melatonin user.
Lastly: I would NOT take high-dose melatonin (or any melatonin for that matter) if a pharmacist or medical doctor thinks it’s a bad idea – such as because it: (A) interacts with current treatments for a specific medical condition; (B) exacerbates a specific medical condition (e.g. depression); or both.
Are high doses and megadoses of melatonin toxic to the body?
No (in most cases). In fact, high doses seem to protect the body to a greater extent against cytotoxins and neurotoxins as a result of more potent anti-oxidative and anti-inflammatory actions.
According to some researchers: “The lethal dose 50 (LD 50) of melatonin is reported to be infinity; i.e., it is impossible to administer a large enough dose of melatonin to kill an animal.” (R)
There’s probably a “sweet spot” type dosing range wherein “more” melatonin might be disadvantageous, counterproductive, or offer such a diminishing return (e.g. such a small additional reduction in oxidative stress relative to dosage increase) – that it makes no sense to administer more.
There is one study I found in which high-dose melatonin was worse than low-dose melatonin with regard to preventing aminoglycoside ototoxicity.
(Apparently super high-dose melatonin causes vasodilation which delivers more of the circulating toxin to the ears.)
Any potential negative side effects from high-dose melatonin?
Taken consistently (e.g. nightly) over a long-term, high-doses of melatonin could be detrimental to performance (physical and/or cognitive) and may adversely modify levels of specific hormones.

Some even think that high dose melatonin shrinks testicles during pubertal development.
Individuals with slow CYP1A2 metabolism and/or impaired liver/kidney function are more likely to experience adverse events or more pronounced reactions following high-dose melatonin – particularly if administration is chronic (e.g. every night for weeks/months).
- Circadian dysregulation: In persons who are poor CYP1A2 metabolizers and/or those with impaired melatonin clearance – high-dose melatonin may dysregulate the circadian rhythm. Even in those who don’t metabolize melatonin slowly, administration for several days may still disrupt the circadian rhythm if the dose is high enough.
- Melatonin accumulation: Melatonin may accumulate within the body quicker than excreted – particularly in persons with CYP1A2 slow metabolism; users of certain medications that affect melatonin kinetics; and/or those with kidney and/or liver impairment.
- Atherosclerosis (?): In hypercholesterolemic mice with an atherogenic diet, supplementation with melatonin highly increases the surface of atherosclerotic lesions in the proximal aorta. (R) Though this is an animal study (involving mice) and cannot be directly extrapolated to humans, it’s possible that certain people (e.g. those with hypercholesterolemia) will react similarly to high-dose melatonin.
- Eye damage (?): A study in rats found that melatonin treatment increased light-induced damage to photoreceptors (in the eyes) – whereas pinealectomy protected photoreceptors from light-induced damage. (R) Although it’s unclear as to whether similar effects occur in humans, the possibility should be considered – particularly among high-dose melatonin users.
- Autoimmune conditions (?): A study in mice found that melatonin exerts an immunostimulatory effect which exacerbated both the onset and severity of collagen-II arthritis (CIA) – a model of rheumatoid arthritis (RA). (R) Though we cannot assume the same outcome for humans, the possibility warrants consideration in persons with susceptibilities.
- Depression (?): Individuals with depression can experience a worsening of depression from melatonin at low and normal doses. High doses of melatonin may significantly exacerbate depressive symptoms and should be used only with extreme caution (assuming necessary) in those prone to depression.
- Brain fog, cognitive deficits, fatigue (?): High-dose melatonin levels can significantly raise daytime plasma concentrations of melatonin in some individuals – and if the dose is high enough, it does it in everyone. Consequences are multi-fold: brain fog, cognitive deficits, fatigue/lethargy, grogginess, etc. – all during the day.
Will high dose melatonin cause tolerance?
Probably not. There’s no evidence from scientific studies of long-term (months/years), daily melatonin administration at reasonably high doses (e.g. 10-15 mg) indicating that tolerance occurs.
Read: Melatonin Tolerance.
The one caveat here is that there may be some threshold dosage at which tolerance does occur (on average or for a majority of users) with consistent long-term melatonin administration.
Perhaps melatonin tolerance was never reported in scientific literature is because either: (A) dosage wasn’t high enough [for tolerance induction] OR (B) study duration wasn’t long enough [to observe tolerance].
If you’re using 50-100 mg melatonin per night, it’s fair to assume that there could be increased risk of developing tolerance relative to lower doses.
Assuming melatonin tolerance is a legitimate phenomenon, higher doses will induce more significant tolerance (relative to lower doses).
Note: It is important to distinguish between “tolerance” and circadian dysregulation.
- Just because melatonin no longer works after a consistent period of administration does NOT mean that its lack of effect is due to “tolerance.”
- (In most cases – it’s actually due to excessive systemic melatonin accumulation.)
Which individuals might benefit most from high-dose melatonin?
Included below are individuals that I suspect might benefit more from high-dose melatonin than others.

(Keep in mind that this is mere speculation – and not based in any strong science.)
CYP1A2 rapid metabolizers
I hypothesize that CYP1A2 rapid metabolizers will tolerate high-dose melatonin well – such that it may actually be better (up to a certain dose/threshold) than low-dose melatonin.
This hypothesis is based on the finding that CYP1A2 poor metabolizers accumulate melatonin significantly at even standard doses such that it can dysregulate the circadian rhythm.
Because rapid metabolizers (CYP1A2) metabolize melatonin extensively, it may reduce bioavailability and increase elimination – hence some logical justification for high-dose use.
Caffeine users
In many cases, caffeine interferes with sleep architecture and quality (even if it isn’t subjectively noticed by the sleeper).
It does this by preventing adenosine from binding to adenosine receptor sites – and modulating core components of cellular “clocks” (increasing cyclic AMP).
If the caffeine intake is substantial – higher-dose melatonin might help some caffeine users by increasing nighttime melatonin signal strength substantially (following substantial signal blunting as a result of the caffeine).
In my experience, higher doses of melatonin work better than low doses for both induction and maintenance of sleep following caffeine intake.
That said, melatonin does NOT directly counteract caffeine’s psychoactive effect (on adenosine receptors) – so do not assume it’ll always work.
Read: How to Counteract Caffeine.
Sleep maintenance insomnia sufferers
Low-dose and standard-dose melatonin supplements are generally adequate for induction of sleep (decreasing sleep onset latency and managing primary insomnia.)
However, high-dose melatonin has been hypothesized to be better for management of maintenance insomnia (i.e. wake up and can’t fall back asleep).
The rationale of high-dose melatonin for sleep maintenance insomnia is as follows: (1) higher doses deliver higher systemic concentrations of melatonin; (2) melatonin concentrations remain higher for longer durations (relative to lower doses); (3) maintaining higher melatonin levels for longer durations may help sustain sleep (as melatonin tends to induce drowsiness).
Gooneratne et al. (2012): High-dose (>2 mg) melatonin (sustained-release) recipients maintained melatonin levels >50 pg/mL for ~10 hours – whereas low-dose (<0.5 mg) melatonin (sustained-release) recipients exhibited elevated melatonin levels for ~6.4 hours. (R)
Low dose-melatonin led to a 7-fold increase in melatonin peak levels (from baseline) – whereas high-dose melatonin led to a 65-fold increase in melatonin peak levels (from baseline).
Unfortunately, Gooneratne et al. did NOT record/document: sleep quality, sleep architecture, etc. – so we don’t know whether high-dose melatonin is actually superior for maintenance insomnia.
Excessive light exposure at night
Recent studies show that indoor room light (500+ lux) strongly suppresses melatonin and phase shift responses. (R)
Translation: Regular light exposure at night reduces melatonin levels and disrupts circadian rhythms. These effects are synergistic with caffeine – such that caffeine intake plus light exposure at night suppress melatonin to a greater extent than either as a standalone.
Assuming melatonin is suppressed significantly from light exposure – it may be possible to overcome or attenuate some of the resulting adverse effects with high-dose melatonin supplementation.
High systemic inflammation
High-dose melatonin likely exerts a significantly more potent anti-inflammatory action than low-dose melatonin.
Therefore, higher doses are probably superior for the management of high systemic inflammation (at least over a short-term) – relative to lower ones.
Some experts believe a melatonin dosage of 500 mg/night may be useful in the treatment of “cytokine storms” (i.e. bouts of incredibly high inflammation) as a reaction to COVID-19. (R)
In conditions like Duchenne Muscular Dystrophy (DMD) which are associated with high inflammatory reactions, high-dose melatonin (60 mg/night + 10 mg/morning) seems to provide significant benefit (as observed by bloodwork).
In sepsis (i.e. life-threatening complications from infection), high-dose melatonin probably works significantly better than lower-dose melatonin.
Hardeland (2021) suggests that melatonin doses up to several hundred milligrams may be ideal for sepsis. (R)
High oxidative stress
High-dose melatonin likely exerts a significantly more potent anti-oxidative action than low-dose melatonin.
Therefore, higher doses are probably superior for the management of high oxidative stress (at least over a short-term) – relative to lower ones.
The reduction in oxidative stress from high-dose melatonin (60 mg/night & 10 mg/morning) has been directly observed in patients with Duchenne Muscular Dystrophy, as evidenced by reductions in plasma lipid peroxidation (LPO) and nitrites (No(x)) – markers of nitrosative/oxidative stress. (R)
Hardeland (2021) suspects that a substantial reduction in oxidative stress from high-dose melatonin may prove therapeutic in sepsis and viral diseases. (R)
Specific medical conditions/scenarios…
- Mild neurodegeneration
- Specific cancers
- Amyotrophic Lateral Sclerosis (ALS)
- Duchenne Muscular Dystrophy (DMD)
- Sepsis & infections (e.g. TB, COVID-19, Influenza)
- Nerve injury/damage
- Undergoing surgery (e.g. liver surgery)
- Hearing loss
- Tinnitus coping
- Autoimmune conditions
- Stroke recovery
- Drug dependence & addiction
Who should NOT use high-dose melatonin consistently?
I’m not the authority on who should use (or avoid) melatonin.
If you aren’t sure whether melatonin is a good fit for you – talk to a medical doctor.

Below are specific cohorts that I suspect (based on research I’ve read) will not react well to high-dose melatonin (10+ mg) – particularly if administered consistently (i.e. daily) for a significant duration (e.g. weeks/months).
- Slow CYP1A2 metabolizers: Those who are slow CYP1A2 metabolizers (this is genetic) will accumulate high-dose melatonin if its administered regularly for more than several weeks. This accumulation will dysregulate the circadian rhythm and worsen sleep. For these individuals, lower doses (0.3 mg or lower) are optimal.
- Pediatrics & adolescents: There may be potential alterations in hormone levels and puberty onset, etc. Assuming a young person benefits from melatonin, using the minimal effective dose is something I’d recommend (range: 0.3 mg to 10 mg at most).
- People with “brain fog” or cognitive impairment: Higher doses of melatonin will increase daytime sleepiness in many cases, which in turn will exacerbate brain fog and cognitive impairment. If you already have brain fog – be cautious about melatonin.
- Users of other substances: High-dose melatonin may be more likely to: (A) interact with; (B) potentiate; (C) be potentiated by – co-administered substances and generate adverse effects. Talk to a medical doctor and pharmacist to determine a safe melatonin dose for you.
- People with depression: A majority of people with depression will react adversely to high-dose melatonin (such that it’ll exacerbate depressive symptoms). This will be particularly apparent if the depressive subtype consists of slowed thinking, low arousal/anxiety, and lethargy/fatigue.
- Overweight & obese: Yes – melatonin can help some people with sleep… and getting good sleep can help with weight loss. However, research suggests that very high doses of melatonin may cause overeating and weight gain.
- Select autoimmune conditions: Melatonin likely has potential to be beneficial to a subset of persons with autoimmune conditions – yet detrimental to another subset of persons with autoimmune conditions. Immunology is incredibly complex. I’d recommend working with an immunologist and have some bloodwork analyzed to evaluate how melatonin is affecting your immune system if you have an autoimmune condition and plan to use a high-dose of melatonin consistently.
- Hormonal abnormalities: At normal “high” doses, melatonin probably shouldn’t cause significant changes in hormone levels (in most users). That said, everyone responds differently – and select people may be susceptible (for whatever reason) to hormonal changes from melatonin supplementation. Megadoses of melatonin (e.g. 500-1000+ mg), particularly when administered on a daily basis, are more likely to affect hormones. High-dose melatonin users should get hormones checked at regular intervals to ensure no unhealthy changes ensue.
- Previous bad experience(s): Obviously if you’ve responded poorly to high-dose melatonin in the past, it’s probably a sign that your body doesn’t tolerate it well (for whatever reason). For example, if you experienced depressed mood after using low-dose melatonin – the depression might be even more significant if you were to use high-dose melatonin.
- Melatonin receptor variants: Persons with certain variants of melatonin receptors (MT1 & MT2) may be more likely to experience unfavorable reactions/adverse effects from high-dose melatonin than those with other variants. (Variation in the expression of melatonin receptors hasn’t been sufficiently researched to predict/examine variant-specific reactions to high-dose supplementation.)
Note: Although high-dose melatonin may significantly reduce inflammation (in some cases/users), this does NOT mean that all medical conditions with high inflammation somehow significantly benefit from melatonin.
(Example: Someone with depression has high-inflammation. High-dose melatonin may lower the inflammation but alter neurochemistry in a way that significantly worsens depressive symptoms.)
Furthermore, a subset of medical conditions may be accompanied by systemic inflammation as a therapeutic reaction (rather than something that’s causing/worsening the condition.)
Note: If you aren’t sure whether high-dose melatonin is ideal for you – talk with a medical doctor and pharmacist (to determine potential effects on health, medical conditions, and potential interactions with other substances you use).
What if you benefit from melatonin but can’t tolerate a high dose?
Simple don’t take a high dose. Instead? Take the “minimum effective dose” (MED).
This refers to the lowest possible amount of melatonin to achieve a therapeutic/beneficial effect.
(MED is a pharmacological concept – the lowest dose level of a pharmaceutical product that provides a clinically significant response in average efficacy.)
Credit Tim Ferriss for popularization of the phrase – as he’s who taught me.
If for whatever reason you need a high dose, you should work with a medical doctor and pharmacist to ensure you’re limiting potential dangers/downside.
What about other melatonin formats & modes of administration?
This article (and its referenced dosages) focus primarily on high-dose orally-administered melatonin.
However, as I’ve mentioned, orally-administered melatonin (in most formulations) exhibits extremely low bioavailability.
Overall, it’s likely that novel melatonin formats and/or non-oral modes of melatonin administration could significantly increase bioavailability and intraneural activity such as to exert effects similar to high-dose oral melatonin, from much lower doses.
Melatonin formats: It’s possible that, in the future, someone figures out how to bind/pair melatonin with another chemical such as to massively increase its bioavailability and/or uptake specifically into the brain/CNS.
(This has been done with curcumin paired with piperine, magnesium bound to threonic acid a.k.a. threonate, etc.)
Preliminary research shows that melatonin added to nano-sized carriers significantly increases bioavailability relative to standard formulations. (R)
Modes of administration: Sublingual, intranasal (i.e. inhaled), subcutaneous, transdermal, and intravenous routes of administration likely exhibit significant pharmacokinetic differences relative to oral melatonin.
For example, sublingual and intranasal formats of melatonin might bypass first-pass metabolism and deliver significantly more biologically active melatonin per milligram – than oral melatonin.
Note: Just wanted to write this section so that readers know “high doses” of oral melatonin may provide similar effects to low dose sublingual or intranasal melatonin (due to higher bioavailability for the latter modes of admin.)
Which high dose melatonin supplement do I recommend?
I like Pure Encapsulations Melatonin 20 mg for immediate-release (IR) format.
The main reason I like Pure Encapsulations is that they don’t have any additives or “fillers” in the supplement – just melatonin.
However, I’ve found many other formats of melatonin to work well such as:
- Nature Made Melatonin 10 mg: Can simply double, triple, quadruple, etc. dosing as needed for higher dose.
- Natrol Melatonin (10 mg XR): Beware this contains B6 & calcium.
- NOW Melatonin 10 mg: Works well for me.
It’s probably best to calculate the cost per mg ($/mg) and figure out which company has the best deal per milligram.
(Then simply take more capsules if lower dose increments cost less per milligram).
If your primary focus is convenience – go for 20-60 mg capsules.
Note: The above are affiliate links. Cost is the same whether you use my links or not. By using the links you help support the site.
Have you ever taken high-dose melatonin?
- What effects have you experienced from high-dose melatonin? Were they beneficial or deleterious?
- Why were you taking high-dose melatonin?
- Did you work with a medical doctor and get bloodwork done?
- Have you noticed any significant changes in cognitive function or physical performance as a result of high-dose melatonin supplementation?
- What was the dose?
- One time (i.e. single dose), short-term (e.g. 1-4 weeks); or long-term (e.g. months/years)?
- What were the effects of high-dose?
- Any other substances you took with the melatonin?
Thank you for sharing all this research!
This article is the best I have found on Melatonin so far.
Thank you :)