Just last year I developed Eustachian tube dysfunction after intentional weight loss via a combination of caloric restriction and physical exercise. It took me awhile after experiencing my first episode of Eustachian tube dysfunction before actually discovering that it was likely caused by (relatively rapid) weight loss. Below I’ve documented my history with weight loss-induced Eustachian tube dysfunction, as well as various interventions that have helped me get it under control – these days I know how to completely prevent dysfunction.
Anyways, before you get too far down in the article, I wanted to break a few things down for the sake of general knowledge.
What are Eustachian tubes?
Small tubes positioned between your middle ears and upper throat. The function of these tubes is to equalize pressure within your ear, as well as drain fluid from your middle ear (the region of the ear behind your eardrums). In most cases, these tubes remain closed – except when chewing, swallowing, or yawning. (That’s why when dysfunction occurs, people often try to chew, swallow, yawn – hoping that it’ll normalize things).
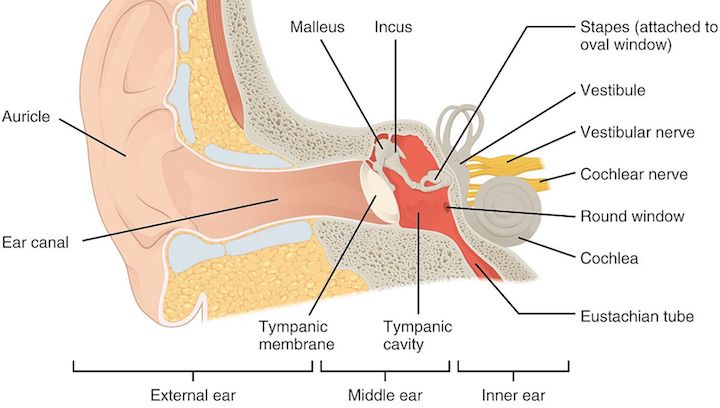
Image credit: OpenStax Anatomy & Physiology
What is Eustachian tube dysfunction?
Eustachian tube dysfunction refers to abnormal function of the Eustachian tubes. In other words, the Eustachian tubes aren’t functioning properly. This can cause a variety of unpleasant symptoms for the person affected such as: autophony, hearing problems, pain, and/or tinnitus. In many cases, Eustachian tube dysfunction resolves on its own, however, some individuals with the condition may require surgical intervention for tube normalization.
Eustachian tube dysfunction from weight loss?
First, to be clear, many people who lose weight do NOT experience any Eustachian tube dysfunction following their weight loss. That said, weight loss is a very common cause of Eustachian tube dysfunction. The type of Eustachian tube dysfunction most associated with weight loss is referred to as “Patulous Eustachian tube.” Those experiencing Patulous Eustachian tube will have their tubes remain “opened” instead of “closed.”
Peritubal atrophy: The chief cause of Eustachian tube dysfunction after weight loss is atrophy of peritubal adipose tissue. During weight loss (or fat loss), the body metabolizes fat from within the ear (peritubal adiposity). Because this peritubal adiposity supports the Eustachian tubes, when fat is lost, the open/close function of the tubes is impaired, often manifesting as Patulous (open) Eustachian tube.
There are other potential adjunctive causes of ETD after weight loss, but peritubal fat loss is likely the primary driver. Potential adjunct causes are listed below in the article, but may include things like: dehydration, stimulant use, hormone imbalances, intense exercise, and/or nutritional deficiencies.
Weight Loss & Eustachian Tube Dysfunction (Research)
While researching weight loss and Eustachian tube dysfunction, I conducted a simple PubMed search to find some studies that might be worth discussing. Unfortunately, although it’s widely accepted among medical professionals that weight loss causes Eustachian tube dysfunction, there’s very little quality research on the topic. My search revealed just a couple articles that I deemed relevant and/or informative enough to discuss.
It is my hope that there will be future research conducted in attempt to estimate the prevalence of ETD after weight loss – within the general population. Additionally, I should note that I suspect many people who lose weight and develop ETD never report it – or even suspect that it’s from their weight loss. Even if these individuals accurately determine that it’s from their weight loss, they probably won’t go through proper medical channels (e.g. otolaryngologists) for accurate diagnosis and/or an explanation that weight loss was the cause.
2017: Patulous Eustachian Tube Dysfunction: Patient Demographics and Comorbidities.
A recent publication documented the efforts of Ward, Ashry, and Poe (2017) who examined a large cohort of individuals with Patulous Eustachian tube dysfunction. They compiled data from medical reports of outpatients who presented with Patulous Eustachian tube between 2004 to 2016. Researchers discovered a few things about sufferers of Patulous Eustachian tube:
- Majority female: 54% of sufferers were female – slightly more women were affected.
- Age of onset: Average age of symptom onset was 38 years.
- Common symptoms: Autophony, aural fullness, tinnitus, crackling sounds (in that order).
- Symptoms: Increased in frequency and duration over time, were aggravated by exercise, and improved with adjusting head position (dependent position), sniffing, respiratory infection, and ipsilateral internal jugular vein compression.
- Bilateral vs. unilateral: Approximately 52% of sufferers had problems in both ears.
- Comorbidities: Allergies was the top comorbidity (49%), but weight loss was second (35%). Laryngopharyngeal reflux (33%), anxiety (31%), autoimmunity (13%), and neuromuscular disease (8%) were also causes.
- Weight loss-induced ETD demographics: Among sufferers of weight loss-induced ETD, average weight loss prior to onset was ~43.43 lbs. (19.7 kg). Most patients were older, accurately/rapidly diagnosed, and had persistent symptoms.
- Treatment: Most patients responded well to medical treatment (53%), but others (47%) required surgery.
(Reference: https://www.ncbi.nlm.nih.gov/pubmed/28796094)
2014: The Impact of Acute Loss of Weight on Eustachian Tube Function
An article by Pascoto, Abreu, Silva, Weber, Pignatari, and Stamm (2014) is currently the most relevant in regards to weight loss-induced Eustachian tube dysfunction. The group of aforementioned researchers evaluated the frequency and intensity of Eustachian tube dysfunction symptoms in a group of obese patients following bariatric surgery.
- 19 obese patients: A total of 19 patients with obesity were included in this research – none of whom had a history of ear disease or ear surgery.
- Bariatric surgery: All patients underwent bariatric surgery. Bariatric surgery is a procedure in which the size of the stomach is reduced via utilization of a gastric band, via removal or a portion of the stomach, or via rerouting the small intestine to a small stomach pouch.
- Hearing questionnaire: All patients underwent a hearing evaluation and questionnaire: prior to surgery, on the day of surgery, 3 months post-surgery, and 6 months post-surgery. The evaluations included an: otoscopy, tonal/vocal autiometry, and impedanceometry.
- Pre-surgery: None of the 19 patients experienced Eustachian tube dysfunction symptoms prior to surgery.
- After surgery: Following surgery, 5 patients (26.3% of the sample) exhibited Eustachian tube dysfunction symptoms at the first post-operative evaluation. At the 6-month follow-up evaluation, 9 patients experienced symptoms of Eustachian tube dysfunction (47.3%).
Researchers in this study concluded that bariatric surgery can cause symptoms of Eustachian tube dysfunction. It was suggested by researchers that the Eustachian tube dysfunction was likely due to a combination of rapid weight loss and loss of peritubal fat.
(Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4296987/)
My own case of weight loss-induced Eustachian tube dysfunction
Though I’ve experienced the occasional clogged Eustachian tube from viral infections (e.g. the common cold) and seasonal allergies, I had never experienced Eustachian tube dysfunction until fall of 2016. When I had my first episode of Eustachian tube dysfunction, I was convinced that some pathogen(s) had been circulating throughout my body and somehow got into my ear canal. I was convinced that these pathogens were going to ultimately damage my inner ear and cause sensorineural hearing loss (thankfully this never happened).
In time, I realized that there probably wasn’t a virus or bacteria colonizing in my ear canal. After doing some thorough research of my own, as well as consulting multiple medical doctors, I concluded that my ear issue was a form of Eustachian tube dysfunction known as Patulous Eustachian tube. This occurs when the Eustachian tube remains opened instead of staying closed. In my case, the cause of my Patulous Eustachian tube was a byproduct of rapid weight loss – and possibly less significant adjunct variables such as: my diet (macros/micros), caffeine intake, and high stress.
Introduction: I want to preface this section by providing a recap of my bodyweight fluctuations prior to the onset of my Eustachian tube dysfunction.
From 2011 to 2013, I was doing a combination of Crossfit, P90X, Insanity, and marathon training – I ran my first marathon and finished with a pretty good time considering that, prior to this marathon, I had never done any long-distance running. During this period my bodyweight hovered at around 165 lbs. I was in great cardiovascular shape, ripped with substantial muscle definition, but was not overly bulky or massive. I looked like an athlete rather than a bodybuilder.
In 2013 I got the idea that I wanted to switch up my workout routine and do some bodybuilding. I ran a 5-day split at my gym for the next year and was pleased with the results. During this period, I was essentially on a perma-bulk – eating well-above my maintenance level of calories. I gained a solid amount of muscle during this year, but I also gained a moderate amount of fat. Because I enjoyed the routine and muscular appearance, I continued the bodybuilding-style routine and diet.
Although in retrospect I’m not sure why I did this, I set a goal for myself of reaching 200 lbs. bodyweight. At some point in early 2015 I reached my 200 lb. bodyweight goal but felt overweight and uncomfortable so I dropped weight relatively quickly (and easily). Thereafter I would maintain a bodyweight that hovered between 185 lbs. and 188 lbs. for the remainder of 2015 and 2016. Though unnecessary to mention, I also switched from bodybuilding to powerlifting – and powerlifted for about a year before transitioning to a minimalistic workout routine for the sake of occupational productivity.
Recap: My bodyweight increased from 165 lbs. to 200 lbs. and then dropped back down to about 185 lbs. Although I added a significant amount of muscle to my frame during this period, I also added a lot of fat. During these periods in which my bodyweight shifted, I had zero problem with my ears – zero Eustachian tube dysfunction.
7-day water fast: Influenced by an episode of SmartDrugSmarts (a podcast) featuring Dr. Thomas Seyfried and later by an episode of the Tim Ferriss Show featuring Dominic D’Agostino, I forced myself to try a 7-day water fast in Fall 2017. (The aim of this fast is to kill precancerous cells throughout the body that are reliant upon glucose for fuel. With fasting there are a number of mechanisms by which precancerous cells may die).
Although the fast was difficult for me (especially the first few days), I didn’t experience any major adverse reactions. My only side effects during the fast were: hunger (obviously), low energy (duh), impaired cognition (due to hunger), orthostatic hypotension (this is common), and some minor lightheadedness. After the fast my bodyweight had dropped over 10 lbs. – from above 180 lbs. to about 170 lbs.
To be clear, this was very rapid weight loss. Some of the weight loss was obviously water, but the rest was fat. In the second week after my fast, I resumed a normal diet and reinstated my simplistic workout. It was during one of these workouts that I noticed a crackling sound within my ears and a felt a sudden suction-like sensation within my ear canal. I thought this might’ve been due to some latent virus and/or bacteria that resurfaced during my fast.
In addition to the crackling and suction-like sensation, my right ear felt sealed up and unable to hear sounds from the outside. I constantly yawned and swallowed – hoping that my ear would unclog. Although my ear unclogged within the first 10 minutes after my workout, I was afraid of any potential hearing damage from pathogens. I spoke to my brother about this and he suggested that my experience might be due to a clogged Eustachian tube.
At this point I didn’t know nor care because the ear normalized. Thereafter I continued experiencing some inner ear crackling and intermittent suction-like sensations in my ears (usually just one ear at a time). These episodes were most common during or after my workouts – and would spontaneously resolve within 30 minutes of completing my workout.
Though I had never experienced these ear issues prior to my water fast, I figured that they were somehow tied to exertion. In my mind I suspected that my ear issues were a result of latent infections that resurfaced during the 7-day water fast and damaged my inner ear. I was somewhat depressed about this thought, but figured that I could live with the symptoms as long as they only occurred when exercising.
More weight changes: After my water fast, I didn’t see a point in maintaining my new weight. I gradually regained all of the weight that I lost during the fast and continued hovering around 185 lbs. without any further “ear episodes.” That said, during the winter I began following a high protein, high carbohydrate, low fat diet for weight loss. A few fitness YouTubers that I watched were starting a cut during January/February/March and I wanted to follow suit. I adhered to a cutting diet for approximately 1.5 months and lost approximately 10 lbs.
Cold night’s walk (Episode #1): A night in late February I went for a long walk (about 45 minutes) outside in the snow to clear my head – I was highly stressed from work. My body felt run-down due to a combination of lifting weights, poor sleep, and a caffeine crash. Though the first half of my walk was pleasant, I noticed some crackling in my ears.
I figured it must be the same crackling that I experienced after my water fast. I continued assuming that this inner ear issue was caused by an opportunistic latent pathogen that circulated throughout my body during the water fast. Anyways, because my sinuses were plugged during my walk, I engaged in “snot rocketing” to clear them.
One of these snot rockets induced a vacuum-like sensation within my right ear followed by tinnitus (ringing) and inability to hear external sounds. It felt like a vacuum sealed my ear shut and I experienced substantial autophony – perceiving loud self-generated sounds like my breathing and heartbeat. I immediately panicked – jumping up and down, yawning, yelling, and contorting my head/neck in attempt to unclog the ear.
Unfortunately, none of my actions helped and I assumed the worst – sudden-sensorineural hearing loss. I debated going to the emergency room for corticosteroids, but it was late and I figured that it may improve by morning. In effort to protect my ear, I administered Vitamins A, C, E + Magnesium – a combination believed to help minimize (and sometimes prevent) ototoxicity. Though I was still panicking as a result of the inner ear suction-like sensation and compromised hearing ability, I forced myself to relax by using paced breathing to decrease sympathetic tone (i.e. the stress response).
I slept pretty well that night and woke up the next morning feeling much better. Though I couldn’t tell whether my ear had normalized, it felt at least 90% better than before I fell asleep. By the end of the following day, I had convinced myself that it was probably 100% recovered and would continue to improve. Nonetheless, I debated scheduling a doctor appointment for antibiotics and/or antivirals – as I thought this was caused by a pathogen.
Research: I discussed the episode with my brother who suggested that it was probably my Eustachian tube. I didn’t believe him and feared the worst case scenario. I also thought that if I saw a standard medical doctor (rather than an ENT), I would receive an improper diagnosis such as cerumen impaction (i.e. earwax buildup) so I avoided doctors. Instead I endeavored to conduct research for an accurate self-diagnosis.
Initially I looked for correlations between water fasting and ear problems on Google. I couldn’t find much of anything. Next I searched for possible latent infections that may disseminate (spread throughout the body) during fasting. I searched whether bacterial or viral infections would most likely inflict damage during a water fast… (turns out viral infections are poorly controlled while fasting – whereas bacterial infections tend to significantly improve).
I looked up various types of viruses and debated (again) scheduling a doctor’s appointment to attain a prescription for antiviral medications. I continued searching PubMed and Google, but wasn’t really that convinced with my initial hypothesis of a disseminated virus inflicting inner ear damage during/after a water fast. Eventually I searched for what my brother suggested – Eustachian tube dysfunction.
After reading about Eustachian tube dysfunction, I figured that this was a viable possibility. That said, I was not yet convinced that this diagnosis was accurate. It wasn’t until I thought about the fact that I had lost weight that I decided to search for the terms “weight loss” and “Eustachian tube dysfunction.” From here I uncovered anecdotes of individuals who developed a condition known as Patulous Eustachian tube after losing weight.
I then glossed over some general information regarding Patulous Eustachian tube and realized that the symptoms matched perfectly with my experience.
Intentional weight gain: Because one of the first-line treatments for Patulous Eustachian tube is weight gain, I immediately stopped my weight loss diet and deliberately gained weight as fast as possible. After regaining weight, all inner ear issues ended and Eustachian tube function normalized. No Eustachian tube dysfunction occurred at my elevated bodyweight. Because I’d much rather be overweight than deal with the madness that is Patulous Eustachian tube, I maintained this weight and was satisfied – I still fell within a “healthy BMI.”
Weight loss: I stopped thinking about weight loss and maintained my pre-weight loss homeostasis of 185 lbs. until summer. In early Summer 2017, I wanted to attempt weight loss again and determine whether the Eustachian tube dysfunction would reemerge. I lost weight at a rate of 1-2 lbs. per week and had no Eustachian tube problems in the process. By late June I weighed just under 170 lbs. and had zero Eustachian tube dysfunction.
Family reunion (Episode #2): In early July I was attending a family reunion at which I knew there would be a large meal for dinner. I fasted the entire day and, just an hour before the dinner, I opted to lift some weights and do some cardio. Towards the end of my lifting session, while doing heavy dumbbell shrugs, my right ear went from perfect to clogged.
This induced significant anxiety, and once again, I wanted to rush to the emergency room or an ENT. I took my usual stack of supplements and did my best to cope while eating dinner with family that I hadn’t seen in years. My hearing was completely distorted for most of dinner and I found it very difficult to enjoy myself. Because I figured it was Patulous Eustachian tube, I ate like an absolute pig, hoping that the ad-libitum feeding would help my ear.
Though my Eustachian tube was dysfunctional for the remainder of the night, it had normalized by the following morning. Nevertheless, I didn’t want to experience another episode during the reunion so continued eating large portions of food with plenty of dietary fat. By the end of the reunion I had packed on a few pounds, but my Eustachian tube caused no further problems.
Self-analysis: When this second episode of Eustachian tube dysfunction occurred, my bodyweight was between 165 lbs. and 170 lbs. Furthermore, I had been consuming caffeine regularly, intermittent fasting, exercising vigorously (often while fasted), and had followed a “low fat” diet. I also may have been slightly dehydrated and/or had some micronutrient deficits.
After gaining weight and experiencing no further Eustachian tube dysfunction, I maintained a weight between 170 lbs. and 178 lbs. I’m currently around 175 lbs. Since my episodes of Eustachian tube dysfunction, I’ve tinkered with my weight a few more times and have come to the realization that dropping below 170 lbs. significantly increases likelihood of my Eustachian tube dysfunction. While I hadn’t ever experienced Eustachian tube dysfunction at a weight of 165 lbs. in the past, I hadn’t ever gained a significant amount of weight before reaching 165 lbs. (only lost a slight amount).
The fact that I reached 200 lbs. and then maintained 185 lbs. for several years likely altered the size and/or anatomical layout of my inner ear. Even a slight alteration as a result of the increased adipose pressure (from a heavier weight) could’ve facilitated a permanent stretch/change. This may explain why I’m more likely to experience intermittent Eustachian tube dysfunction at the weight of 165 lbs. – a weight at which I never experienced any Eustachian tube issues.
I should also mention that my Eustachian tube dysfunction is usually intermittent and short-lived. That said, I’d rather have a slightly higher body fat if I can avoid the dysfunction as even one episode is seriously disconcerting – causing substantial psychological stress for its duration. For this reason, I now maintain as low of a body weight as possible – but not too low as to avoid Eustachian tube dysfunction.
Why does Eustachian tube dysfunction occur after weight loss?
Though I’m no expert, I’ve developed some hypotheses regarding how Eustachian tube dysfunction occurs during/after weight loss. Understand that my hypotheses are based upon a combination of scientific literature and my own thoughts (self-reflection). Moreover, you should realize that the specific weight(s) of causal factors may differ among individuals who experience Eustachian tube dysfunction after they lose weight.
Hypothesis: Inner ear adiposity changes to cause Eustachian tube dysfunction after fat loss
When I deliberately gained weight to reach 185 lbs. via bulking for bodybuilding, this probably increased fatty tissue (peritubal fat) around my Eustachian tubes. The increased adiposity probably provided increased pressure around the tubes to remain closed. When I dropped down from 185 lbs. to 165 lbs., my hypothesis is that the Ostmann fat pad (adiposity around the Eustachian tube) shrunk and may have been a different shape than it was during my pre-bodybuilding days at 165 lbs.
As a result of the shrinkage, there’s less support to maintain closure of my Eustachian tubes and I experience unwanted opening. Gaining a bit of weight back provides some additional support for the tubes via increased adiposity and helps maintain closure.
An analogy to help explain Eustachian tube dysfunction after weight loss
To help explain Eustachian tube dysfunction after weight loss, I’ve thought of an analogy. (This analogy is far from perfect, but may help you better understand what might be happening). The analogy involves elastic sweatpants. When you’re at a light bodyweight and a new pair of elastic sweatpants fit well, the elasticity should stay tight around your waist.
Now, hypothetically, let’s say you gain a bunch of weight (20+ lbs.) and continue wearing the same sweatpants over an extended duration (e.g. several years). The elasticity of the sweatpants will stretch out to accommodate your new bodyweight. Your increased bodyweight and bigger waist size are increasing pressure on the elastic strap of the pants and stretching them out.
Similarly, if you gain weight from a light bodyweight, the fatty tissue around your Eustachian tube increases. This extra fatty tissue puts additional pressure on your Eustachian tube and provides more support for closure (which prevents unwanted opening). Later, let’s say you decide that you want to lose the 20+ lbs. that you originally packed on.
You go on a low calorie diet, increase your activity, and/or have weight loss surgery – the weight comes off. Now that you’ve lost the weight that you gained, the same sweatpants may be too stretched out for a proper fit – your waist has shrunken and there’s less pressure to support the elastic strap. As you wear the pants at your lighter weight, you may notice that they occasionally fall down – sometimes unexpectedly.
Similarly, after your weight loss, the fat mass around your Eustachian tubes shrinks – and there’s less support for the tubes. As a result of this inadequate support for the Eustachian tubes, one or both may have difficulty closing – or accidentally open; lack of support impairs the open-close mechanism. Inevitably, just like the sweatpants randomly fall down after weight loss (due to no longer fitting your waist), your Eustachian tubes may randomly stay open (instead of closed) due to lack of adipose support.
In some cases of weight loss, the adipose support around the tubes may be so inadequate, that Eustachian tube dysfunction is chronic (rather than intermittent); akin to the sweatpants being so stretched out that they no longer fit. Moreover, because significant fatty tissue surrounded the tubes at your heaviest (fattest) weight, this may have “stretched” out the area or altered the internal anatomy – creating a wider gap between the fat cells and Eustachian tube.
This is what I believe happens to a person’s Eustachian tube during/after significant weight loss. Essentially the anatomy of the adiposity surrounding the Eustachian tube has changed and lacks pressure to keep the tube closed – so it sometimes slides open and is problematic. When a bit of weight is regained, adiposity increases around the Eustachian tube and provides more support – similar to the fact that your stretched out sweatpants would fit better (and be less likely to fall) if you regained some of your lost weight.
Understand that not everyone will necessarily experience this condition after substantial weight loss due to other factors (e.g. inner ear anatomy), but many do. Additionally, my guess is that this effect of weight loss often goes underreported because those experiencing Eustachian tube dysfunction do not understand it. They may suspect that it’s due to “allergies” or a “cold” or just think something weird is happening to their ears from excessive cerumen (i.e. wax).
Secondary hypotheses: Fat storage genetics, Macros, Micros, Recalibration
In addition to my primary hypothesis for the cause of Eustachian tube dysfunction after weight loss, I’ve developed a few secondary hypotheses – some of which could be adjunctive to the primary hypothesis and each other. Secondary hypothetical causes of Eustachian tube dysfunction from weight loss include: fat storage genetics, macronutrient intakes, micronutrient deficits, physiologic recalibration, and stressors.
Fat storage genetics: Most experts understand that genetics regulate the storage of adipose tissue throughout the body. Individuals with certain genes will store more weight around their hips, whereas others might store less weight around their hips and more weight in their buttocks. Because genes regulate distribution of fat throughout the body, they probably also influence where fat will be “mined” (lost) from the body during weight loss.
Two individuals at the same height, weight, and body fat may go on the exact same diet – with the same number of calories. They both may lose a similar amount of fat, but the fat loss may occur in different areas. One individual may lose significantly more fat from the area around the Eustachian tubes whereby he/she develops Eustachian tube dysfunction after weight loss, whereas the other individual may not lose much (or any) fat around the Eustachian tubes from weight loss.
This may fully (or partly) explain why certain individuals are more likely to develop Eustachian tube dysfunction after weight loss – than others.
Macronutrient deficits: While on a weight loss diet, most individuals limit intakes of specific macronutrient groups such as: carbs, proteins, and fats. Though it’s certainly possible to lose weight with a balanced intake of macronutrients, certain individuals may restrict one particular macronutrient more than others. In many cases, those dieting will restrict their intakes of fats while keeping protein and carb intakes high.
Restricting fats may be more likely to cause Eustachian tube dysfunction than restriction of other macronutrients. In part, this may be due to the fact that extremely low fat diets often interfere with normative hormone production. Hormonal imbalances associated with extremely low fat diets may alter interstitial pressure within the ear canal whereby they induce Eustachian tube dysfunction.
Another possibility might be that low fat diets yield delays and/or alterations in distribution of adiposity during weight loss. Because fat is most efficient of all macronutrients for the body to store as energy within adipose tissue, higher intakes of fat while restricting calories to lose weight may be superior for maintenance of fatty tissue that supports Eustachian tube function. While carbs will eventually get deposited as fat, the potential of delayed storage and/or altered distribution may cause Eustachian tube dysfunction.
It may be similarly possible that extreme low carbohydrate and/or low protein diets also cause Eustachian tube dysfunction during weight loss for other reasons. Extreme low carb might also interfere with hormone production and extreme low protein may cause muscles within the inner ear to atrophy. If you’re limiting the intake of any particular macronutrient, it’s possible that it might’ve played a role in your Eustachian tube dysfunction.
Micronutrient deficits: While losing weight, many individuals fail to monitor their micronutrient intakes. A good insurance policy for micronutrient deficits is a standard multivitamin, however, not everyone thinks to purchase multivitamins. Failure to monitor micronutrient intake and/or malabsorption of micronutrients could result in a deficiency – perhaps a major one. The only way to confirm a hypothesized deficiency (or multiple deficiencies) is via bloodwork.
Assuming someone who’s recently lost weight exhibits a micronutrient deficiency, it’s possible that this deficiency would interfere with normative functions of the inner ear. This interference may play a role in triggering Eustachian tube dysfunction. Perhaps if the micronutrient deficiency is reversed such as via dietary alterations and/or supplementation, function of the Eustachian tubes would normalize.
Recalibration phase: It’s possible that during and/or immediately after weight loss, the Eustachian tubes and/or supporting structures are subject to a recalibration of size. Perhaps during weight loss, the Eustachian tubes lose adiposity faster than other areas of the body. However, when a person attains his/her new healthy bodyweight and maintains it for an extended duration, adiposity may gradually increase and/or the Eustachian tube anatomy may adapt such that the dysfunction abates.
Moreover, increasing caloric intake as a result of weight maintenance (compared to weight loss) calories may help with normalization of Eustachian tube function. That said, if I had to bet, I’d say that this hypothesis is likely to be inaccurate for a majority of sufferers due to the fact that many individuals manage to maintain their lower bodyweight for a long-term yet their Eustachian tube dysfunction persists.
Stressors: Experts have suggested that stress may play a direct or adjunct role in the pathogenesis of Eustachian tube dysfunction. For some individuals, getting stress under control is enough to normalize Eustachian tube function. During weight loss (especially if rapid), individuals are under a significant amount of physical and psychological stress.
It is known that the body increases production of stress hormones (e.g. cortisol) while cutting weight – the body doesn’t like to shift away from homeostasis. In addition to increased production of stress hormones during weight loss, many endeavoring to lose weight will increase physical activity such as by jogging or lifting weights which further stresses the body. If a person is deficient in macronutrients or micronutrients, this adds to the cumulative load of stress.
A bit of psychological stress from dietary restriction, usage of stimulants (e.g. caffeine), a tough day at work, and/or poor sleep – and you’re suddenly highly stressed out. Perhaps stress and/or stress hormones can alter interstitial pressure within the ear and induce Eustachian tube dysfunction during/after weight loss.
List of influential variables for ETD after weight loss
Included below is a list of all variables that I consider important influencers in the onset of Eustachian tube dysfunction after weight loss. Keep in mind that more research is needed to elucidate the primary and secondary drivers of ETD after weight loss. I’ve endeavored to list variables in order by hypothesized degree of influence. As of current, I believe the 3 most influential variables in causing Eustachian tube dysfunction after weight loss include: total weight (fat) loss, inner ear anatomy, and fat storage genetics.
- Total fat loss: I believe the single biggest cause of Eustachian tube dysfunction associated with weight loss is the total amount of fat a person loses. While most research suggests that general weight loss causes Eustachian tube dysfunction, this is probably because weight loss is usually associated with fat loss. Technically, someone who loses muscle mass (e.g. a bodybuilder who retires) may experience significant weight loss – but most of this weight loss will have been from muscle (not fat) and probably won’t lead to Eustachian tube dysfunction. In any regard, persons who lose a substantial amount of body fat are at increased risk of developing Eustachian tube dysfunction. This is because when a person loses a significant amount of fat, the fat surrounding the Eustachian tubes will decrease whereby pressure/support needed to promote closure is reduced.
- Inner ear/nose anatomy: Another likely influencer of weight loss-related Eustachian tube dysfunction is inner ear anatomy. Many people who lose substantial body fat after long-term morbid obesity will never develop or experience Eustachian tube dysfunction. For this reason, it’s likely that the specific anatomical layout of a person’s inner ear dictates whether Eustachian tube dysfunction presents after weight loss. Perhaps structural variations of inner ears (specifically the middle ear canal) and/or nose either: completely protect against, reduce likelihood of, or increase likelihood of – weight loss-related Eustachian tube dysfunction.
- Fat storage genetics: Also not farfetched is the idea that genetics associated with body fat storage predict whether Eustachian tube dysfunction (after weight loss) occurs. It is known that areas of body fat storage can differ significantly among individuals – some people store more fat in their lower abdomen, others in their hips, and others in their buttocks. Similarly, during weight loss, a person may lose weight from certain regions quicker than other regions – and these regions can vary based on the specific individual. Knowing this, it’s possible that certain genes might increase storage of fat around the Eustachian tubes during substantial weight gain (to stretch out and/or alter anatomy), but when the weight is lost, Eustachian tube dysfunction occurs due to the [potentially permanent] weight gain-induced anatomical changes. Others may not be subject to as much (or any) fat gain within the inner ear, possibly explaining why they don’t experience Eustachian tube dysfunction after losing weight.
Other possible triggers of weight loss-related ETD
Though the total amount of fat loss, inner ear anatomy, and/or fat storage genetics are likely causally-implicated in ETD after weight loss, other variables may play a role. These include things like: duration of obesity, speed of weight loss, nutrition, stressors, hydration, and physiologic recalibration.
- Duration of obesity: It’s possible that the duration over which a person is obese (storing too much body fat) plays a small role in determining whether ETD occurs after weight loss. If someone gains a significant amount of weight for a short-term (e.g. a few days or weeks), it’s possible that the anatomy around the Eustachian tubes won’t be subject to lasting alterations. Perhaps quick reversion to a healthy body fat percentage from short-term obesity preserves normative inner ear anatomy. However, if obesity is maintained for a long-term (e.g. years), anatomy around the Eustachian tubes may be permanently altered and unable to normalize after weight loss.
- Speed of weight loss: It’s also possible that the speed at which someone loses weight might determine whether Eustachian tube dysfunction occurs. Someone who loses 3-5 lbs. per week might be more prone to significant fat metabolism within the inner ear than someone who loses weight gradually at a pace of 0.5 lbs. per week. It’s also possible that rapid weight loss doesn’t give the inner ear and/or Eustachian tubes enough time to adapt/adjust to functioning with reduced adiposity. Gradual weight loss may allow or guide the inner ear and/or Eustachian tubes to slowly acclimatize to functioning at a lower weight. Moreover, rapid weight loss can alter hormone levels, increase stress, and increase likelihood of dehydration – each of which might affect interstitial pressure within the middle ear to induce Eustachian tube dysfunction.
- Nutrition: It is known that deficiencies in macronutrients and micronutrients can deleteriously affect many biological processes. It’s possible that someone on an extreme diet in which fats, proteins, or carbs are restricted – might be at increased risk for developing ETD. Going with an extreme low fat (in particular) might be most problematic in that hormone levels may significantly shift. Furthermore, because dietary fat is deposited more efficiently as adipose than other macronutrients, a low fat diet might limit and/or alter adiposity around Eustachian tubes to increase odds of dysfunction. Any deficiencies in micronutrients could also affect physiological processes associated with Eustachian tube function such that likelihood of ETD increases.
- Stressors: Simply losing weight is known to significantly upregulate production of stress hormones. Any increase in the production of stress hormones might alter interstitial pressure within the middle ear and increase likelihood of ETD during weight loss. While dieting, many individuals are stressed about cutting calories and/or may be using stimulants (which further increase stress) to suppress appetite. Individuals may also be putting their body under additional stress with increased physical activity in the form of cardio and/or weight lifting. All of these stressors could trigger and/or increase odds of ETD from weight loss.
- Dehydration: When losing weight, it may be easier for persons to end up dehydrated. During the first week of a diet, most people lose a few pounds of “water weight.” Additionally, because many people attempting to lose weight are exerting themselves physically via cardio and lifting, it’s easy to become dehydrated. Add some stimulants to the weight loss equation (e.g. caffeine), many of which facilitate a diuretic effect – and it’s even easier to become dehydrated. Dehydration is a widely-recognized trigger (and potential cause of) ETD in a subset of persons.
- Smoke exposure: If you’re a smoker or exposed to any form of second-hand smoke such as from other smokers or a wood-burning fireplace, you may be at increased risk of developing Eustachian tube dysfunction after weight loss than others. Regular inhalation of smoke can alter many biomarkers and downstream physiologic processes – one of which could be the Eustachian tubes.
- Allergies: Allergies alone can trigger Eustachian tube dysfunction in some persons. If your ETD didn’t occur until you lost significant weight, then fat loss is probably the primary cause. Still, if you’re exposed to any allergens, these may augment fat loss in causing your ETD after weight loss.
Choosing between being skinny with ETD and fat without ETD?
If you develop Eustachian tube dysfunction after weight loss, you may feel as though you traded one problem for another – the excessive body weight for an inner ear disorder. In the event that your Eustachian tube dysfunction is severe and incessant after weight loss, you’ll probably be willing to regain all of your lost weight to reverse the condition. In the event that your Eustachian tube dysfunction is barely noticeable and/or intermittent after weight loss, you’ll probably be willing to live with it because you’re now at a healthier/attractive weight.
Making a choice: Let’s say you need to choose between Eustachian tube dysfunction and being overweight – which should you pick? If it were me, I’d take being overweight in a heartbeat because I know how disconcerting and psychologically-stressful Eustachian tube dysfunction can be. When my attacks occurred, I was so stressed out that I couldn’t even think straight. Moreover, I experienced a seriously uncomfortable vacuum-like sensation within my inner ear. So if I had to choose for myself – I’ll take being slightly fat over Eustachian tube issues.
- Severe ETD: Those experiencing severe ETD (intense/nonstop) after weight loss should probably regain lost weight. Severe ETD may damage hearing over time and most with severe ETD will be subject to significant psychological distress (anxiety/depression). For this reason, it’s best to reverse the condition as quickly as possible via weight gain.
- Moderate ETD: Those experiencing moderate ETD (fairly intense/regular) after weight loss may wish to regain lost weight. Even moderate ETD such as experiencing dysfunction twice per week can cause significant psychological distress and feel very unpleasant. For this reason, weight gain is probably a good idea.
- Modest ETD: Those experiencing modest ETD (less intense/infrequent) after weight loss may wish to maintain their lighter weight. Modest ETD may be preventable by avoiding triggers such as stress, dehydration, and overexertion. Moreover, you probably won’t be bothered enough by the transient bouts of dysfunction to deliberately gain weight.
If there’s absolutely nothing you can do to control your Eustachian tube dysfunction after weight loss and it’s driving you crazy, you’ll probably want to regain some weight. My recommendation would be to regain just enough weight to make it stop – this quantity will differ for everyone. Don’t jump all the way back up to your peak obese weight, but gain a little bit so that your Eustachian function normalizes.
Other ETD management options: That said, there’s a chance that you won’t need to choose between ideal body weight and Eustachian tube dysfunction. For some people, Eustachian tube function might normalize after the body is given enough time to fully adapt to a lower weight. If the body never adapts to the lower weight, it may be best to maintain the low weight (for the sake of health) and undergo Eustachian tube surgery.
- Recalibration: Another thing to consider is that there might be some sort of physiologic hangover/layover after weight loss in which the body (and inner ears) require time for adaptation to the new lower body weight. Perhaps after weight loss is complete, calories can be increased slightly (to maintenance) whereby the adiposity of the inner ear increases to normalize Eustachian tube function. It’s also possible that when weight loss is complete and maintained for an extended duration, the inner ear structures undergo recalibration and adapt to the lower body weight such that Eustachian tubes eventually normalize from their acute dysfunction.
- Surgery: If you want to stay at a lighter body weight after weight loss, yet don’t want to deal with ETD, you may want to undergo surgery. Various types of surgeries can be performed to promote closure of the Eustachian tube. In most cases, surgery is safe without significant side effects and is effective for ~50% of patients.
As I mentioned, if I had to choose between Eustachian tube dysfunction and being overweight, I’d take being overweight. Furthermore, I would probably only use surgery as a “last resort” such as if my only options were: healthy weight with ETD and morbid obesity without ETD. For most people though, including myself, there’s probably some “middle ground” that can be attained in which weight remains fairly healthy and Eustachian tube function is normal.
For example, if I lost 60 lbs. from 200 lbs. to reach a weight of 140 lbs. but experienced weight loss-related ETD, I’d likely try gaining weight gradually until the condition abated. When the condition abated, I’d attempt to determine the cutoff weight at which likelihood of ETD increases. Assuming the ETD never occurs at any weight above 150 lbs., I could simply gain 10-15 lbs. and hover between 150 and 155 lbs. to prevent further ETD.
Even if this new weight is higher, as long as it’s within a healthy BMI, I’d be satisfied. Even if it was slightly overweight (based on BMI), I’d opt to maintain this slightly overweight BMI if it meant normal Eustachian tube function without the need for surgery. However, if I needed to regain all of my lost weight (and revert back to morbid obesity) for normalization of Eustachian tube function, I’d probably opt to stay at a lighter body weight and inquire about surgery. Ultimately, it’s up to you to decide how you’d like to manage your Eustachian tube dysfunction after weight loss.
How to Minimize Likelihood of Eustachian Tube Dysfunction from Weight Loss
As of current, there are no scientifically-substantiated ways to decrease likelihood of Eustachian tube dysfunction from weight loss. Those who experience Eustachian tube dysfunction from weight loss probably were at greater risk due to their amount of weight gain (more weight gain may yield greater anatomical change), anatomical layout (your anatomy may increase/decrease likelihood of ETD), and genetics (particularly those involved in fat storage and metabolism). Below are some hypothesized steps you could take that might decrease your odds of Eustachian tube dysfunction from weight loss. Usefulness of these suggestions may be subject to individual variation.
- Gradual weight loss: It may be possible to prevent Eustachian tube dysfunction with gradual weight loss. I’ve hypothesized that, for some persons, rapid weight loss may mine an increased amount of adiposity from areas around the Eustachian tubes compared to gradual weight loss. While the final outcome may be the same (when ideal body weight is reached), perhaps gradual weight loss preserves adiposity within the inner ear better than rapid weight loss and/or allows the Eustachian tubes to gradually recalibrate to decreased adiposity – whereby dysfunction never occurs. For the sake of definition, gradual weight loss would be within the range of 0.25 lbs. to 1 lb. per week.
- Evaluate diet: It is recommended to evaluate your diet to ensure that you’re getting adequate macronutrients and micronutrients. You should be consuming enough carbohydrates, fats, and proteins – as deficiencies in any particular macronutrient could alter physiology in ways that might be problematic for your Eustachian tubes. Of all macros, I believe that adequate fat is most important for prevention of Eustachian tube dysfunction during weight loss. Going too low on fat may result in inadequate storage of fat within your ear and/or alter interstitial pressure within the ear to induce ETD.
- Reduce stress: Because stress may trigger (or directly cause) ETD in a subset of individuals, it’s best to limit stress as much as possible if you want to avoid ETD. A variety of effective methods for stress reduction include: ceasing use of stimulants (e.g. caffeine), avoiding overexertion (e.g. excessive exercise), meditating/deep breathing, getting adequate sleep, and/or using anxiolytics. Any stress increase puts you at elevated risk of developing ETD.
- Hydration: Staying hydrated is extremely important during weight loss. Hydration helps your body flush out toxins that are released from fat cells as you metabolize longstanding body fat. Moreover, there’s evidence that dehydration (regardless of the cause) may trigger Eustachian tube dysfunction. While you don’t need to water board yourself, drinking the RDA of water for your sex/size may prove to be a helpful prophylactic.
- Supplementation: Unless you’re getting regular blood panels to determine micronutrient levels within your body, you run the risk of a deficiency – especially during a fat loss phase. Though not suggested in the literature, it’s possible that a micronutrient deficiency could play a role in the onset of ETD. Therefore, supplementation with vitamins, minerals, and/or electrolytes may help reduce odds of ETD during weight loss.
What about individuals who lose weight from a starting healthy weight?
Because most persons who experience ETD from weight loss are those who’ve lost weight from an overweight/obese state to reach a healthy weight, it may be informative to highlight persons who develop ETD after weight loss from an already-healthy weight. In other words, someone struggling with a restrictive eating disorder like anorexia nervosa may end up dropping well-below what’s medically classified as a healthy weight such that they end up underweight.
In this case of a person dropping from a healthy weight to an abnormally low weight, if ETD occurs, it’s still caused by underlying fat loss. However, this is generally favorable in that as soon as the individual reaches a “healthy weight,” Eustachian tube function should normalize. Conversely, when an obese person reaches a “healthy weight,” Eustachian tube dysfunction is more likely to occur. (In short, reaching a normal weight for someone who’s underweight should fix their problem, whereas reaching a normal weight for someone who’s overweight may cause their problem).
What do I believe caused my Eustachian tube dysfunction after weight loss?
In my own case of Eustachian tube dysfunction (Patulous Eustachian tube) as a result of weight loss, I suspect that fat loss (around the tubes) was the primary driver. That said, I think that if I would’ve abstained from gained 35 lbs. (much of which was likely fat) to reach 200 lbs. during a bodybuilding phase (from a starting weight of 165 lbs.), I doubt that I would’ve ever developed Eustachian tube dysfunction. I still may have developed Eustachian tube dysfunction if I lost a significant amount of weight from 165-170 lbs., but I could’ve just gained the weight back and things would’ve normalized.
Because I had elevated my weight significantly above homeostasis for an extended duration (maintaining 185 lbs. for years), I believe this slightly altered my inner ear anatomy. When the weight was lost, the slightly altered inner ear anatomy resulted in dysfunction at my previous weight of 165 lbs. Thankfully, my BMI is still considered medically healthy all the way up to 179 lbs., and as long as I stay between 170 lbs. and 175 lbs., I can avoid ETD and maintain decent health.
Although the initial weight/fat gain, maintenance period (several years), and eventual loss probably caused my ETD, I believe that my inner ear anatomy played a role as well. After speaking with an ENT (Ear, Nose, Throat) doctor, I learned that the anatomy of my right ear is slightly abnormal. Predictably, it was this ear that was primarily affected by the Eustachian tube dysfunction after weight loss.
What triggers my episodes of Eustachian tube dysfunction during weight loss?
For me, it seems as though there are some triggers for Eustachian tube dysfunction during weight loss. Although having a bodyweight below 170 lbs. increases likelihood that I’ll experience Patulous Eustachian tube, it doesn’t guarantee it. When I’m under 170 lbs., various things are more likely to trigger ETD. Below is a list of the triggers I’ve observed.
- Intense exercise: Any intense physical exercise can trigger an episode of ETD when below my threshold weight of 170 lbs. I’ve had more episodes occur when lifting heavy weights than when engaged in intense running. This may be related to breath holds under heavy loads. Anecdotally, I’ve also noticed that ETD occurs more when doing shoulder/neck exercises such as: heavy shrugs or weighted neck curls. I have experienced ETD on very fast runs, but these episodes were shorter-lived than after lifting. I should also note that ETD was more likely to occur for me when I performed intense exercise while fasted (13-17 hours).
- Intermittent fasting: Another trigger for my ETD may have been intermittent fasting. Though intermittent fasting helped me control my caloric intake, it seemed as though the longer the fast, the more likely ETD was to occur. If I’d fast for 19 hours, I was more likely to experience ETD than when fasting for just 15 hours. Moreover, if I intensely exercised deep into the fast (e.g. after 18 hours), ETD was more likely to occur.
- Dehydration: Most of the times that I experienced ETD, I was probably slightly dehydrated. I certainly wasn’t “fully dehydrated” or anything like that, but I was probably lacking adequate water intake. Though I don’t believe hydration played a significant role in my ETD, it’s possible that it was an adjunctive trigger.
- Low fat diet: This could be coincidental, but my most severe cases of ETD occurred when following a low fat diet. Though I researched the amount of fat to ensure that it was not below a “safe” quantity, perhaps this altered physiology and/or adiposity of the inner ear to a greater extent than a higher fat diet would’ve. I should note that I experienced a minor ETD episode with a slightly higher fat diet, but a low fat diet seemed to correlate with my most extreme episodes.
- Low calorie diet: To lose weight efficiently, I restrict my calories. Sometimes I restrict below 2000 per day, other times below 1700 per day, and other times below 1500 per day – depending on my activity level. Generally, I realized that the greater the restriction, the more likely I was going to experience ETD. This was probably mostly due to the fact that I reached a lower body fat sooner at the lower caloric intakes, but may have been due to the sheer significance of restriction and/or rapid speed of fat loss.
- Nose blowing: While losing weight and/or maintaining a weight at which I experienced ETD, I found that nose blowing and/or “snot rocketing” could directly trigger an ETD episode. Blowing my nose forcefully was probably the most significant trigger. If I blew my nose lightly, it was less likely to trigger an episode. (I should note that when I’m above 170 lbs., I can blow my nose full force without risking any Eustachian tube abnormalities).
- Caffeine: I’d sometimes drink caffeine late into my intermittent fast and then go exercise. The added stimulation and diuretic effect of caffeine may have increased likelihood of ETD after weight loss as a result of increasing stress hormones and dehydrating the body, respectively. Coupling the caffeine with intense exercise, fasting, and nose blowing – this may have been the perfect storm of ETD triggers.
- High sodium: It seemed as though when I consumed more dietary sodium, ETD was more likely to occur. This could’ve just been a coincidence, but it’s possible that an acute fluctuation in blood pressure and/or ear pressure as a result of high sodium intake may help trigger ETD during weight loss.
How I Manage My Eustachian Tube Dysfunction
If Eustachian tube dysfunction arises, I do whatever I can to get it under immediate control. Thankfully, most of my episodes only last less than 20 minutes, but some have persisted for several hours. For me, the condition is extremely uncomfortable and significantly increases my psychological stress. Below are some steps I take to manage Eustachian tube dysfunction (as caused by weight loss). Do not use any of these strategies without first consulting a medical doctor to ensure safety.
Acute interventions
These interventions may prove useful immediately during/after an ETD attack.
- Immediate caloric surplus: The first and most important thing I do to control my ETD is consuming a caloric surplus. This means eating ad-libitum and zero calorie tracking. If I want unlimited of a particular food – I eat unlimited of that food. I ensure that I’m getting enough fats (usually from nuts and avocado), then evaluate carbohydrates and proteins. The purpose of the caloric surplus is to increase fat within the ear. Next, I maintain this surplus for as long as necessary to get my ETD under control. Even if the ETD subsides, I continue eating more calories just to be on the safe side.
- Supplements: The next thing I do is administer a cornucopia of supplements. I personally use the combination of Vitamins A, C, E + Magnesium which has been suggested to reduce oxidative stress within the ear and facilitate an otoprotective effect. I may also use a multivitamin to ensure that I’m not deficient in any other micronutrients. Sometimes I’ll take ALA and krill oil to further decrease oxidative stress and inflammation, respectively. While I’m not sure whether these supplements help Eustachian tube function, I figure they can’t hurt – so I go overboard here.
- Hydration: After supplementing, I drink at least 2-4 full glasses of water. The water is to ensure that the supplements are easier for the body to absorb and/or to prevent them from getting stuck in the GI tract. Because dehydration can cause ETD, the extra hydration may even help reverse dysfunction within the Eustachian tubes.
- Adjust head position: Lying down on your back may help fix dysfunction within the Eustachian tubes. Others have noted that bending forward (from a standing position) until the ears are between the knees/legs may normalize Eustachian tube function. Try modifying your head position – as this may improve your ETD.
- No stimulants: Absolutely zero stimulants are consumed after an episode of ETD – stims are thought to trigger attacks.
- Minimize sodium: I always minimize sodium after an episode of ETD – sodium might alter inner ear functions.
- No exercise: Absolutely ZERO physical activity (lifting, jogging, walking) is done until ETD normalizes. I’ve found that continuing a workout with ETD can make it worse.
- No fasting: Because I suspect that intermittent fasting might trigger ETD for me, I stop intermittent fasting after an episode. My fasting window is reduced to 13 hours – instead of 16-21 hours.
- Nasal spray: My doctor prescribed (Rx) a nasal spray to use when my Eustachian tubes are acting up. Coincidentally, this doctor had experienced the same problem himself at one point and could relate to my experience. Though I’ve used the spray, I didn’t find it very helpful, but figured it didn’t do any harm. I believe it was a steroidal nasal spray, but am not sure of its specific name. Many people find nasal sprays helpful for acute management of ETD – talk to your doctor for a prescription.
Ongoing management
These strategies may prove useful in the days or weeks after an episode of Eustachian tube dysfunction.
- Weight gain: Because Eustachian tube dysfunction after weight loss is likely mediated mostly by reduced body fat around the tubes, an effective way to reverse the condition is via weight gain. Weight gain is easily accomplished by consuming more calories than your body expends (via BMR + exercise) throughout the day. Although weight gain is an effective long-term management strategy for weight loss-induced ETD, you don’t want to go overboard here. It’s recommended to gain just enough weight so that the Eustachian tube dysfunction ceases – but no more. In other words, if you only need to gain 5 lbs. for the ETD to end, don’t go crazy and pack on 30 lbs. Most individuals with weight loss-induced ETD will likely have a “threshold weight” such that, as long as they stay above this weight, Eustachian tube function will remain normative. It may take some self-experimentation to find the lowest possible weight that you can maintain without experiencing dysfunction. For me, my ETD threshold is 170 lbs. – as long as I gain enough weight to reach 170 lbs. and maintain a weight between 170 lbs. and 175 lbs. – likelihood of Eustachian tube dysfunction is virtually nonexistent.
- Daily hydration: In addition to weight gain, another thing that I do to minimize likelihood of Eustachian tube dysfunction attacks is keep tabs on my daily hydration. Dehydration is suspected as a direct cause and/or trigger of ETD in many individuals, including those who experience ETD after weight loss. For this reason, as a precautionary step in potentially preventing another episode of dysfunction, I’ll ramp up my water intake. I typically drink 1-2 large glasses upon waking, have water before and/or with each meal, and then more before bed. Though I’m unsure about the efficacy of maintaining adequate hydration as a prophylactic for ETD – but it can’t hurt so I always drink plenty of water to prevent further episodes. (If you’re unsure about whether you’re drinking enough – review CDC nutrition recommendations. Also understand that hydration is good, but excessive hydration is bad – you shouldn’t be racing to the bathroom every 5 minutes).
- Limit intense exercise: Intense physical exercise is known to trigger Eustachian tube dysfunction in a subset of individuals. I know for a fact that intense exercise can trigger ETD in myself when I’m below my threshold weight of 170 lbs. I’ve experienced ETD during intense cardio (running several miles as fast as possible) and while performing bodybuilding exercises that stimulate the shoulders/traps (e.g. shrugs). Whenever I’m experiencing ETD, I generally reduce or cease all intense exercise. If I want to continue getting some physical activity, I’ll do some extremely light activities like walking or the elliptical until the tubes normalize.
- No stimulants: Research indicates that stimulants may cause and/or trigger ETD via numerous mechanisms including: increasing stress hormones, altering blood flow, and/or dehydrating the body. Because I don’t want to risk another ETD attack, I stop using/consuming stimulants for at least 2 to 4 weeks after an ETD episode. The only stimulatory substances that I consume regularly include: dark chocolate (90% Lindt) and green tea (I make a fairly potent brew). Occasionally (e.g. once every couple months) I’ll have a zero-calorie caffeinated beverage (e.g. energy drink or diet soda). Anyways, absolutely no stimulatory substances will be consumed until I’m convinced that my Eustachian tubes have normalized and are no longer prone to dysfunction.
- Stress reduction: This goes hand-in-hand with cutting out stimulants from your diet. Stress can alter blood flow to your inner ears, hormone levels, and dehydrate the body. For this reason, if whenever I experience weight loss-mediated ETD, I first attempt to manage my stress. It’s hard to keep stress low in the aftermath of an attack (ETD makes me panic), however, it’s probably beneficial to do so. Personally, I try to either meditate OR use paced breathing at least 2 times per day (once in the morning and once at night) to keep stress hormone levels low. I’ll also engage in some relaxing exercise during the day (e.g. walking), take hot showers, and ensure that I’m getting a good night’s sleep. Additionally, I’ll sometimes administer anxiolytic supplements (on an “as-needed” basis) such as: adaptogenic herbs, CBD oil, and magnesium.
- High-fat diet: In my personal experience, it seems as though I’m more prone to Eustachian tube dysfunction after weight loss when consuming a lower fat diet. Although I always ensure that I’m consuming adequate fat during to maintain adequate hormone levels, in my personal experience, I’ve noted a correlation between lower fat consumption and ETD. (Keep in mind that even I’m skeptical of causation here – even after my observation). That said, just in case lower fat diets may increase odds of Eustachian tube dysfunction, I always focus on upping my intake of dietary fat in the aftermath of weight loss-induced ETD. My thought is that because dietary fat gets stored as body fat more efficiently than carbs, it might help minimize duration of preexisting dysfunction. I also know that upping fat intake might aid in the optimization of various hormone levels – which might also favorably influence Eustachian tube function.
- Multivitamin: Another thing that I do for weeks after experiencing weight loss-induced Eustachian tube dysfunction is supplement with a multivitamin. Though not proven in any literature, I believe it’s possible that vitamin deficiencies may directly cause and/or trigger Eustachian tube dysfunction in a subset of individuals during or after weight loss. For this reason, I buy a pack of multivitamins and supplement with one daily for 2 to 4 weeks. (A better thing to do here may be to get a full panel blood test to analyze your vitamin levels, however, this is expensive and may be prone to inaccuracies. Nonetheless, if you identify any specific deficits, it may be better to supplement with those vitamins individual rather than supplementing with vitamins you don’t need – such as would be in a multivitamin).
- No forceful nose blowing: When I’m below my threshold weight of 170 lbs. (and prone to ETD), one thing that triggers an episode of dysfunction is intense nose blowing. Sometimes I’ll “snot rocket” while jogging and this will induce opening of the tubes. Another thing that has triggered an episode is pushing hard while using the bathroom (others have documented this on forums). I always blow my nose very lightly if I suspect that I’m prone to an episode of dysfunction. (After my weight has increased, I can resume normal “forceful” nose blowing).
- Stop intermittent fasting: Though I’m not sure if intermittent fasting could be an adjunct trigger for weight loss-associated ETD, but it’s worth considering. In the weeks after experiencing an ETD episode, I force myself to eat breakfast in the morning and dinner in the evening. I’ll sometimes even have lunch. My purpose for eating at least one meal in the morning and one meal in the evening is to decrease production of stress hormones and provide fuel (which may prevent the body from mining fat stores as would occur in a prolonged intermittent fast). Eating breakfast may be particularly important for ETD sufferers in that a large morning meal can significantly decrease stress hormones (which are known to trigger ETD).
- Avoid extreme weather: Though I’m not convinced that weather conditions increase or decrease likelihood of ETD during or after weight loss, it’s another possibility that I’ve considered. In my experiences, weight loss-related ETD occurred when I was outside (for about 45 minutes) in extremely cold weather and when I was in humid conditions. In the aftermath of ETD from weight loss, I’ll sometimes do my best to avoid extreme weather conditions (hot, cold, humid).
Note #1: Most of the ongoing management strategies that I implement for weight loss-induced ETD are probably less important than fat gain. The fat loss is what likely triggers ETD during/after weight loss (for most). That said, the other things I’ve outlined probably won’t do harm – and may offer substantial benefit as adjunctive interventions.
Note #2: Another thing I’ve never tried is simply staying at my lower body weight for an extended duration to determine if ETD would somehow improve on its own via physiologic recalibration. It’s possible that the ETD may abate once a goal weight is reached and calories are increased to a maintenance level (from a deficit) – possibly restoring adiposity around the tubes to reverse the dysfunction. It’s also possible that physiology eventually “recalibrates” or adapts to the lower weight with enough time (e.g. months, years, etc.) and ETD ceases. Because my episodes of ETD were panic-inducing, I personally wouldn’t want to wait months/years hoping that my physiology somehow recalibrates to correct dysfunctional Eustachian tubes.
Have you experienced Eustachian tube dysfunction after weight loss?
Now that I’ve shared my experience with Eustachian tube dysfunction following weight loss, as well as my hypotheses about what causes it, as well as acute plus ongoing management strategies – I’d love for you to share your experience with ETD after weight loss in the comments section below. Some questions I’d appreciate you answering in your comment include:
- How many times have you experienced Eustachian tube dysfunction after your weight loss?
- What was the duration of each episode that you experienced? What were the worst symptoms?
- Have you been accurately diagnosed by a medical professional (preferably an otolaryngologist)?
- Have you spoken to a medical professional regarding management strategies for your ETD?
- How much weight did you lose before your Eustachian tube dysfunction emerged? (In your lifetime, what was your highest body weight to date?)
- Have you identified a threshold weight at which dropping below increases likelihood of ETD and going above decreases likelihood of ETD?
- Do you believe weight loss/fat loss was the primary cause of your ETD?
- Do you think anything else might have triggered it (e.g. macronutrient/micronutrient deficits)?
- Have you figured out ways to manage your ETD or have you had surgery for it?
- Did you find any of the suggestions within this article helpful for your condition?
- Do you have any suggestions for things that help your weight loss-induced Eustachian tube dysfunction?
(If you leave a comment, don’t feel obligated to answer every question. I’m just trying to identify some commonalities among those who’ve experienced this condition. If some commonalities are identified, this may give more credence to interventions besides simply “gaining weight.”).
Great article! I think I am experiencing the opposite where my tubes stay closed instead of open. I have never had stuffiness in my ears but once I started gaining weight it slowly started happening. My normal body weight I would say is somewhere between 110-120.
I am currently at 145, my highest was 152. I didn’t exercise during this weight gain so it’s surely almost all fat gain. I don’t remember but I think they started feeling stuffed towards the last months of 2021. Now it’s July 2022. The weight gain was quick but not very rapid. Nothing helps my ears and I have tried allergy medication and they are still stuffy.
I pop them regularly by yawning. It’s happening to both ears and sometimes it’s a little worse and sometimes better but they always feel at least slightly stuffy. I think I started noticing the stuffiness when I was around 140 lbs.
Just saw and ENT and he says weight gain has no effect on the ears! I really see no other explanation for this. I am going to undergo an allergy test just in case. But I think the only long term solution will be to lose at least 10 lbs to 15 lbs.
After a series of infections through the summer and winter of 2021 I discovered that I had developed post-menopausal atrophy. My weight went from 197 to 138 lbs.
After getting the atrophy somewhat under control I decided to become a gym shark (even older women like to look good!) and exercised 5 days a week. I maintained a weight of 147, but experienced my Eustachian tubes remaining open (patulous) which was confirmed by my E.N.T.
I have had this condition almost non-stop for 9 months now. There is no prescription which can successfully reverse this condition, saline washes like croing help but only temporarily, and I would save surgery as a last option.
I am now on a higher calorie and fat diet, and have reduced my exercise regime, which will, hopefully, reverse this condition. I am so grateful to the author drewisdope for this much needed information and confirmation of this terrible condition. I am not alone nor am I going crazy!
thought i’d share my experience. since a baby i’ve managed to get myself to 285lb (6’2″ male) in about 30 years. dropped from 285lb to 225lb in about 3 months (2/2020-5/2020) with keto and omad. started getting ETD around 235lb. some days it was all day, other days it was sporadic like only when i went upstairs. i’d say after about 3-4 weeks the ETD went away and lost about another 10lb. been at 225lb now for about 11 weeks, haven’t had ETD. i think for me at least, my own personal opinion, i think i lost fat around the tubes in my head too fast causing them to not stay closed but then my body adjusted and thankfully now i seem to be ok. work out/run now and don’t have issues when exercising. never saw a doctor or anything.
Thanks you for your comprehensive discussion of this topic. I discovered your write up after researching possible causes for my own recently developed, intermittent tinnitus. I am a retired physician (radiologist) with an extensive practice experience of diagnostic imaging in many areas, including disorders of the middle and inner ear. My problem developed recently, after incurring substantial weight loss, while embarking on a “sugar free” or very low sugar diet.
My desire was to effect a healthier long term eating pattern, without the deleterious effects of the added sugar Which is present in so many of our processed foods, and fast food choices. The weight loss was simply a byproduct of this, as I was initially not even monitoring my weight. As I progressed in eliminating sugar laden foods (I was addicted to ice cream, Bluebell, specifically!)
I noticed my clothes becoming very loose. I began to be able to place my clenched fist inside the waist band of my 36 waist size jeans! Therefore I started to monitor my weight. My first weigh in was at about 170, whereas I know I weighed around 187 prior to starting the diet. I have since weighed regularly and gotten as low as 163 lbs. My tinnitus started at about 165 lbs, when I started feeling a fullness in the ears, accompanied by a low pitched “roaring” sound. My ears were free of cerumen, so I was a bit worried, as one of my main hobbies is audio/hi-fi, and I was concerned that I could still enjoy this.
My symptoms were bilateral, though asymmetric, therefore I believed an inner ear tumor, such as acoustic neuroma (schwannoma) was unlikely. My web research led me to the articles you referenced, in which very similar symptoms were reported in a high percentage of patients undergoing bariatric surgery. I then found your lengthy discussion. I did consider proceeding with some medical imaging and auditory testing. I have since consulted with four physician friends of mine, including an ENT specialist.
The ENT doc was somewhat skeptical regarding my self-diagnosis of ETD or Patulous Eustachian tube. My guess is, he may just have not seen this much in practice. Thankfully, my symptoms have spontaneously abated, and I am doing much better, without having to gain weight back. I plan to try to eat more healthy carbs and fats, and stabilize my weight between 165-170 lbs. I am hopeful that my Eustachian tube may have resized itself to the new me, i.e.less peri-tubal fat. I will keep you posted if a different diagnosis is made down the road.
Love the article. I have long had a problem with my ETD. It started when I wanted to become slimmer and went on a very dramatic diet, which was low in carbs and fat. I wasn’t sure it was because of my acute weight loss until I saw the doctor. She advised me nasal spray, but that would only temporarily help. After some online research, I saw that weight gain was the only solution. I gained weight and now I only get episodes when I quickly lose weight. For me, it occurs when I hover around 78 kg, but it can sometimes occur at 80 kg for no apparent reason. I will take your advice and try going on a steady weight loss. When dieting a lot of the time I take it to the extreme, so this time I will make sure not to. Thanks again for the advice. I hope all is well
Thank you so much Drew for sharing your experiences with PET.
I recently developed and recovered from this dysfunction.
My first symptoms of ear popping occurred back in HS football from weightlifting and cardio, but went undiagnosed as there was no explanation for it.
Fast forward to a year ago, I had learned about and implemented the Keto diet along with Intermittent Fasting with great success. My goal was to reach 4-5% BF from starting weight around 220lbs. The heaviest I ever weighed was around 240lbs. Once I worked my way up to fasting for 48hrs, I went the full monty, and decided to water fast till I reached my goal.
I started burning fat at .5lb a day and enjoyed the progress with sustained energy and little appetite. My ears started to pop occasionally though while on the elliptical and increasingly got worse as I lost weight. At my lowest body weight of 157lbs, my right ear would pop consistently after unpopping it, and would stay popped for the whole day till I laid down. That was the point I scheduled an appointment with an ENT which found nothing wrong with my ear.
Only through my own research and experience I came to the same conclusions that you share which are that I lost enough adipose tissue off my Ostmann to cause my ET to stay open. Reluctantly, I started to eat again to prevent chronic symptoms despite my goal. I too didn’t want to gain back all my weight, but would much rather have average weight than have permanent damage as the symptoms are really disconcerting. I wanted to gain back weight from building muscle, but I knew that might not produce necessary fat in my ear, so I went back to eating
Keto with a surplus of calories. Gaining weight back solved the issue. but I wasn’t disciplined about it and gained back up to 190lbs.
Currently, I am back in to extended fasting with the goal to find the lowest BF% I can obtain without symptoms. I think to determine my PET threshold weight, I will include the weight I start to develop symptoms at from the highest heart rate workouts I can achieve. After reaching this threshold weight, I plan to switch to eating a 100 calorie surplus to start building muscle and fill out, but will try to maintain the BF% that the symptoms occur at to see if my ET adjusts to the lack of tissue overtime.
Hi to everyone here. OK I have read about half of your story and sat here nodding away thinking ‘this is me’. Its late here in the UK so will have to keep this short. Since around October 2018 I have dropped from about 23 stones to 19 stones 11lbs, so a loss of about 45lbs. 17lbs of that has been since mid November 2019.
Just before Christmas 2019 I developed distortion in my right ear. Previous to this my only ear problems were impacted wax in 2016 which was resolved by a simple ear syringing. I have seen my General Practitioner who suggested ETD and prescribed a steroid nasal spray. I also have an anxiety/depression diagnosis since aged 20, I’m now 54.
Yes, very comprehensive, interesting, and possibly helpful.
My ETD story doesn’t have the happy weight gain fixes my ETD ending, though. I have been experiencing crackling in my right ear for 5 years, seen 5 ENTs, and have no consensus on what is causing my crackling from any one of them. One said PETD, another said no PETD, for instance.
In 2013, i suffered a nervous breakdown due to extreme life stress (impending divorce, family beak up, chronic pain issues, horrible work problems all at once)
For first time in my life, I fell in to major depressive disorder and generalized anxiety disorder. I lost 35 pounds in about 4 months, going from about 190 to 155 on a 5-9 inch male frame.
The right ear crackling started in March 2014, when I was at my lowest weight. I went in and out of depression and anxiety across next 3 years, gaining, and then losing, 30 pounds again TWICE more.
The ETD — right ear crackling continued no matter what my weight — and it still has continued 2 years after i thankfully pulled out of depression and anxiety.
I bet there is a good chance that my first 35 pound loss — essentially i was so stressed i was barely eating anything, triggered internal ear canal changes that, unfortunately, have continued for me — even at an unhealthy weight of 200 pounds for my 5-9 frame :-(
Anyway, the problem drives me nuts — my right ear crackling is triggered by loud sudden noises such as someone laughing, yelling, loud clanging dishes, silverware, keys rattling, etc and even my own voice, which sucks, because I am a teacher and have to talk/lecture a lot ;-)
I will take a look at maybe eating a higher fat diet, and try less sodium — I LOVE salty foods, and eat a lot of them — and the vitamin combo you suggest. But weight gain is not going to be the thing to fix it for me. I am guessing that for a lot of people, perhaps especially people who have ETD triggered by sudden weight loss caused by something like a major depression and who were at a BMI in mid to upper 20s like me for quite awhile before the sudden weight loss, are probably not going to see the weight gain benefit on ETD that you describe here for yourself.
But I am glad that it works for you :-) — and thank you for sharing your knowledge. I have a youtube video up you can find with a “useless ENTs” google search. It has 18k views in about 2 years. I update my situation in the description below the video youtube.com/watch?v=5826JyW1Dpk&t=9s
Great great article. I think you may have helped me diagnose myself after 6 weeks of doctors/specialists drawing a blank. I have had this problem for 6 weeks now some days worse than others. I lost 8lbs in 2 weeks about 2 months ago to look a little better for my holiday.
Since then my ears have been popping and crackling. I have low tinnitus and I was finding myself stressed an awful lot. The doctors were telling me it may be due to a virus I had gotten over, but now it makes sense due to the timeframe of the illness and my weight loss.
I am now focusing on regaining my lost weight and fingers crossed this sorts my problem out. Thank you so much…
Hi Darren, I am experiencing similar issues after weight loss. Was curious if you had experienced positive results after gaining weight back? It is my intention to gain weight back, however the success rate of this is very limited on the internet. Any help is appreciated.
When I regained my weight the problem slowly disappeared. I recommend foods high in fat and carbs. It worked for me, but it isn’t to say if it will work for you. Best regards.
Thank you so much for taking the time and detail discussing ETD! By far it’s one of the most comprehensive and logical reads I found on the subject! It can get scary out there on the web searching the topic!!
Have you had many people leave comments that they think that weight loss was the cause of their ETD/Patulous? Have they been able to reverse it by putting weight back on?
How are you doing today? Are you still having success keeping it controlled with added weight?
How quickly were you able to gain weight back?
Do you have any tips and recipes to gain weight healthy and quick?
I unintentionally dropped down to 102 from 113 within 7 weeks due to high stress!! Within that time I started getting Patulous. I’d like to get back to 115-118
I appreciate any and all advice!
Hi Christina, similar to my comment above to Darren, I was curious if you had any positive results once you gained back the weight. Thanks!
Hi John, how are your symptoms now?
Hi did your symptoms go away with weight gain?